Tuesday Poster Session
Category: General Endoscopy
P4083 - Impact of Fellow Involvement on Detection of Sessile Serrated Polyps During Colonoscopy
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MB
Mehak Bassi, MD
Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School
New Brunswick, NJ
Presenting Author(s)
Mehak Bassi, MD1, Beatriz Gros Alcade, MD2, Archit Garg, MD3, Aadhithyaraman Santharaman, MD4, Khyati Bidani, MD5, Richa Rani, MD6, Mannat Kaur Bhatia, MD7, Andrew Korman, MD5, Sugirdhana Velpari, MD1, Arkady Broder, MD5
1Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 2Reina Sofia University Hospital, Cordoba, Andalucia, Spain; 3Saint Peter's University Hospital, New Brunswick, NJ; 4Saint Peter's University Hospital/Robert Wood Johnson, New Brunswick, NJ; 5Saint Peter's University Hospital/Robert Wood Johnson Hospital, New Brunswick, NJ; 6Saint Peter’s University Hospital, New Brunswick, NJ; 7Saint Peter's University Hospital/Robert Wood Johnson Hospital, New Brunswick, NJ
Introduction: The Serrated Polyp Detection Rate (SDR) is increasingly recognized as an essential quality indicator for colonoscopy. Multiple studies indicate that the participation of gastroenterology fellows tends to improve adenoma detection rate (ADR). However, only a few studies have assessed SDR during fellowship training.
Our study's objective is to assess the participation of trainees in SDR and ADR throughout their training. This research could significantly contribute to objectively measuring their proficiency in performing colonoscopies.
Methods: We reviewed 1,603 screening colonoscopies (median age 57; 59.4% women) at our institute. Fourteen GI fellows performed 1,025 colonoscopies (63.9%): 201 (12.5%) by first years (F1s), 387 (24.1%) by second years (F2s), and 428 (26.7%) by third years (F3s). We categorized colonoscopy procedures into two groups: attending physicians and fellows (FA) and attending without fellows (A).
Results: After adjusting for confounding variables (Table 1), we observed that the polyp detection rate was higher when GI fellows conducted colonoscopies with attending physicians (Group FA) compared to when attendings performed the procedures alone (Group A) (67.5% vs 54%, p< 0.0001). However, the two groups had no significant differences in the SDR (4% vs 4.5%, p=0.58). The ADR was higher in colonoscopies involving GI fellows and attendings compared to attendings alone (40.6% vs 38.3%, p=0.008).
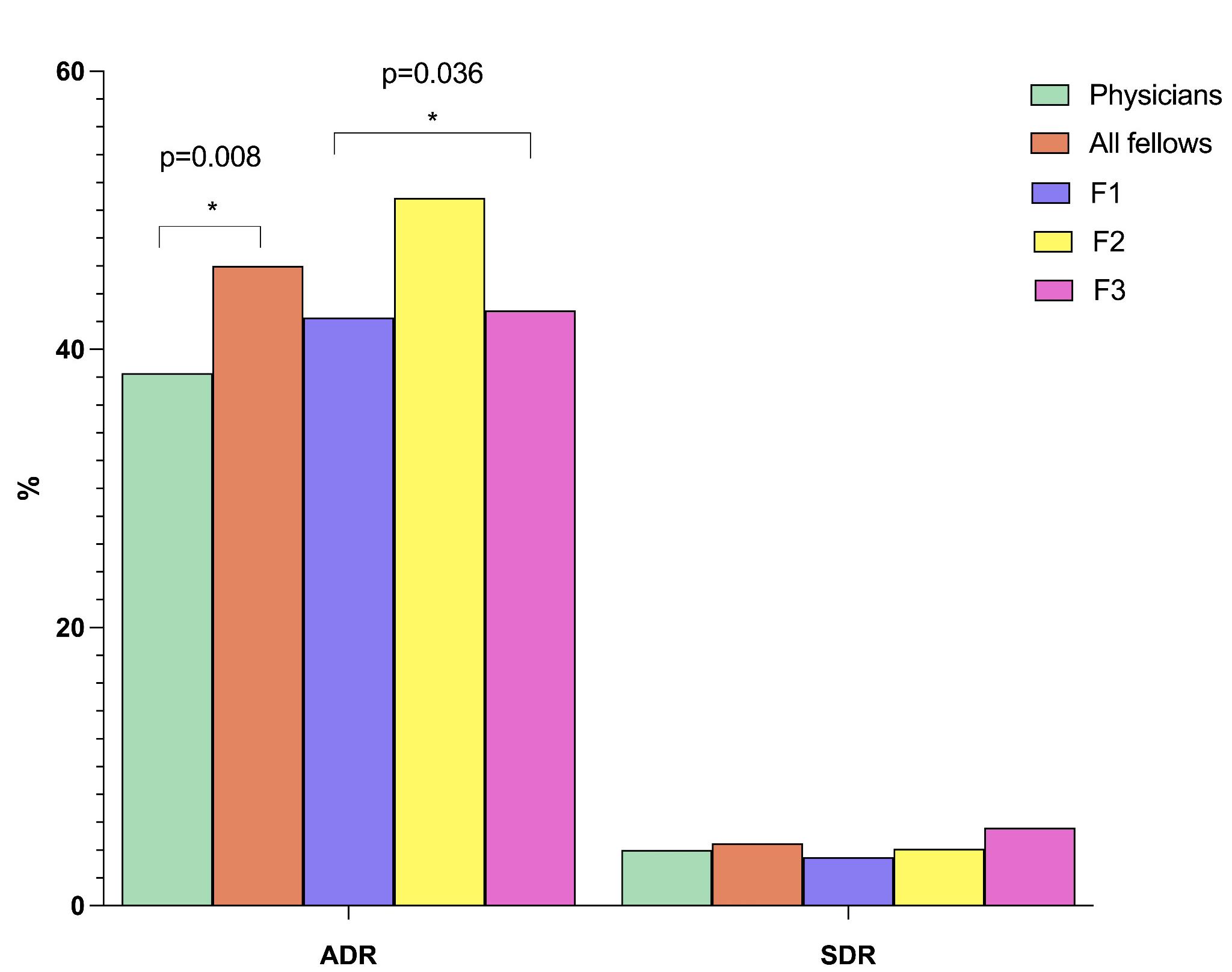
In a subgroup analysis to compare different years of training, we examined the SDR and ADR among first, second, and third years of GI fellows (Figure 1). No significant differences in SDR were found over the three years (3.5% vs. 4.1% vs. 5.6%, p=0.419). However, ADR was higher in the second years compared to the first years (50.9% vs. 42.3%, p=0.036) and in the third years compared to the first years (42.8% vs. 42.3%, p=0.036).
Discussion: These findings suggest that the presence of GI fellows during colonoscopies positively impacted ADR but did not impact SDR. This finding may be attributed to the challenges in detecting these lesions, which are often flat and have a mucous cap, making them difficult to distinguish from the surrounding tissue.
Given that a significant portion of colon cancers arise from the serrated pathway, it is imperative that fellowship training emphasizes correctly detecting these lesions. Our study is one of the few that has assessed SDR with fellowship training, contributing to the limited body of knowledge in this area.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mehak Bassi, MD1, Beatriz Gros Alcade, MD2, Archit Garg, MD3, Aadhithyaraman Santharaman, MD4, Khyati Bidani, MD5, Richa Rani, MD6, Mannat Kaur Bhatia, MD7, Andrew Korman, MD5, Sugirdhana Velpari, MD1, Arkady Broder, MD5. P4083 - Impact of Fellow Involvement on Detection of Sessile Serrated Polyps During Colonoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 2Reina Sofia University Hospital, Cordoba, Andalucia, Spain; 3Saint Peter's University Hospital, New Brunswick, NJ; 4Saint Peter's University Hospital/Robert Wood Johnson, New Brunswick, NJ; 5Saint Peter's University Hospital/Robert Wood Johnson Hospital, New Brunswick, NJ; 6Saint Peter’s University Hospital, New Brunswick, NJ; 7Saint Peter's University Hospital/Robert Wood Johnson Hospital, New Brunswick, NJ
Introduction: The Serrated Polyp Detection Rate (SDR) is increasingly recognized as an essential quality indicator for colonoscopy. Multiple studies indicate that the participation of gastroenterology fellows tends to improve adenoma detection rate (ADR). However, only a few studies have assessed SDR during fellowship training.
Our study's objective is to assess the participation of trainees in SDR and ADR throughout their training. This research could significantly contribute to objectively measuring their proficiency in performing colonoscopies.
Methods: We reviewed 1,603 screening colonoscopies (median age 57; 59.4% women) at our institute. Fourteen GI fellows performed 1,025 colonoscopies (63.9%): 201 (12.5%) by first years (F1s), 387 (24.1%) by second years (F2s), and 428 (26.7%) by third years (F3s). We categorized colonoscopy procedures into two groups: attending physicians and fellows (FA) and attending without fellows (A).
Results: After adjusting for confounding variables (Table 1), we observed that the polyp detection rate was higher when GI fellows conducted colonoscopies with attending physicians (Group FA) compared to when attendings performed the procedures alone (Group A) (67.5% vs 54%, p< 0.0001). However, the two groups had no significant differences in the SDR (4% vs 4.5%, p=0.58). The ADR was higher in colonoscopies involving GI fellows and attendings compared to attendings alone (40.6% vs 38.3%, p=0.008).
In a subgroup analysis to compare different years of training, we examined the SDR and ADR among first, second, and third years of GI fellows (Figure 1). No significant differences in SDR were found over the three years (3.5% vs. 4.1% vs. 5.6%, p=0.419). However, ADR was higher in the second years compared to the first years (50.9% vs. 42.3%, p=0.036) and in the third years compared to the first years (42.8% vs. 42.3%, p=0.036).
Discussion: These findings suggest that the presence of GI fellows during colonoscopies positively impacted ADR but did not impact SDR. This finding may be attributed to the challenges in detecting these lesions, which are often flat and have a mucous cap, making them difficult to distinguish from the surrounding tissue.
Given that a significant portion of colon cancers arise from the serrated pathway, it is imperative that fellowship training emphasizes correctly detecting these lesions. Our study is one of the few that has assessed SDR with fellowship training, contributing to the limited body of knowledge in this area.
Figure: Figure 1: Distribution of Sessile Serrated Polyp Detection Rate (SDR) and Adenoma Detection Rate (ADR) by trainee level, attending with fellows, and attending without fellows.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mehak Bassi indicated no relevant financial relationships.
Beatriz Gros Alcade indicated no relevant financial relationships.
Archit Garg indicated no relevant financial relationships.
Aadhithyaraman Santharaman indicated no relevant financial relationships.
Khyati Bidani indicated no relevant financial relationships.
Richa Rani indicated no relevant financial relationships.
Mannat Kaur Bhatia indicated no relevant financial relationships.
Andrew Korman indicated no relevant financial relationships.
Sugirdhana Velpari indicated no relevant financial relationships.
Arkady Broder indicated no relevant financial relationships.
Mehak Bassi, MD1, Beatriz Gros Alcade, MD2, Archit Garg, MD3, Aadhithyaraman Santharaman, MD4, Khyati Bidani, MD5, Richa Rani, MD6, Mannat Kaur Bhatia, MD7, Andrew Korman, MD5, Sugirdhana Velpari, MD1, Arkady Broder, MD5. P4083 - Impact of Fellow Involvement on Detection of Sessile Serrated Polyps During Colonoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
