Tuesday Poster Session
Category: General Endoscopy
P4084 - The Link Between Trainee Participation in Colonoscopy Procedures and Quality Metrics
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MB
Mehak Bassi, MD
Saint Peter's University Hospital
New Brunswick, NJ
Presenting Author(s)
Mehak Bassi, MD1, Archit Garg, MD1, Beatriz Gros Alcade, MD2, Aadhithyaraman Santharaman, MD3, Khyati Bidani, MD4, Richa Rani, MD4, Mannat Kaur Bhatia, MD5, Babu Mohan, MD6, Arkady Broder, MD1
1Saint Peter's University Hospital, New Brunswick, NJ; 2Reina Sofia University Hospital, Cordoba, Andalucia, Spain; 3Saint Peter's University Hospital/Robert Wood Johnson, New Brunswick, NJ; 4Saint Peter’s University Hospital, New Brunswick, NJ; 5Saint Peter's University Hospital/Robert Wood Johnson Hospital, New Brunswick, NJ; 6Orlando Gastroenterology PA, Orlando, FL
Introduction: Sessile serrated polyps, precursors to about one-third of colorectal cancers, are often missed due to their indistinct borders compared to tubular adenomas. The Serrated Polyp Detection Rate (SDR) is around 5.1% and is increasingly recognized as a key quality indicator for colonoscopy.
While many studies focus on adenoma detection rates by the training year of gastrointestinal fellows, research on detecting sessile serrated lesions during a three-year fellowship is limited. Our objective was to compare the detection rates of sessile serrated lesions (SDR) and conventional adenomas (ADR) across different stages of gastroenterology training.
Methods: We reviewed 1,603 screening colonoscopies (median age 57; 59.4% women) at our institute. Fourteen GI fellows performed 1,025 colonoscopies (63.9%): 201 (12.5%) by first years (F1s), 387 (24.1%) by second years (F2s), and 428 (26.7%) by third years (F3s).
Results: The overall SDR was 4.0%, and ADR was 46% in colonoscopies performed by attending physicians with fellows.
When comparing different years of training (Table 1), no significant differences in SDR were found among F1s, F2s, and F3s (3.5% vs. 4.1% vs. 5.6%, p=0.419). However, ADR was higher in F2s compared to F1s (50.9% vs. 42.3%, p=0.036) and in F3s compared to F1s (42.8% vs. 42.3%, p=0.036). There were no differences in the overall polyp detection rate (tubular adenoma, sessile serrated, and hyper-plastic polyps).
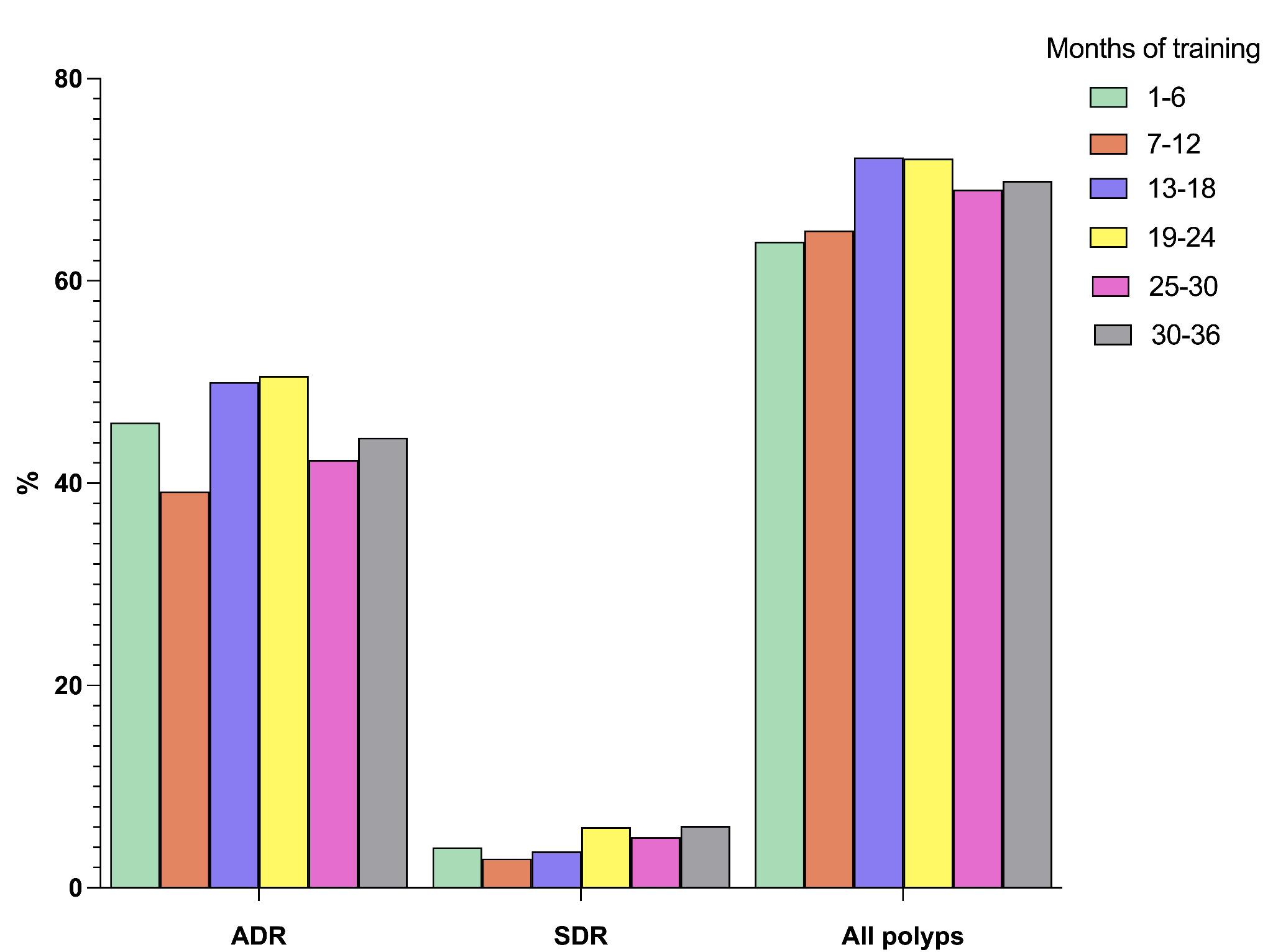
When comparing polyp detection rates by months of training (every six months and beyond), no significant differences were noted in ADR (46.0 vs. 39.2 vs. 50.0 vs. 50.6 vs. 42.3 vs. 44.5, p=0.276) or overall polyp detection rate (63.9 vs. 65.0 vs. 72.2 vs. 72.1 vs. 69.0 vs. 69.9, p=0.590), Figure 1. Similarly, no differences were noted in SDR between different months of training (4.0% vs. 2.9% vs. 3.6% vs. 6.0% vs. 5.0% vs. 6.1%, p=0.730).
Discussion: Our ADR exceeded the national benchmark, but our SDR fell below the recommended quality standard. The overall polyp detection rates and SDR do not show significant variations by year or months of training. Although there is some improvement in specific skills with experience (as seen with ADR in F2s), the overall detection abilities for polyps and sessile serrated remain relatively stable throughout the training period. It may be attributed to the challenges in detecting these lesions, even for board-certified endoscopists. It is imperative that training during fellowship should emphasize correctly detecting serrated lesions.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mehak Bassi, MD1, Archit Garg, MD1, Beatriz Gros Alcade, MD2, Aadhithyaraman Santharaman, MD3, Khyati Bidani, MD4, Richa Rani, MD4, Mannat Kaur Bhatia, MD5, Babu Mohan, MD6, Arkady Broder, MD1. P4084 - The Link Between Trainee Participation in Colonoscopy Procedures and Quality Metrics, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Saint Peter's University Hospital, New Brunswick, NJ; 2Reina Sofia University Hospital, Cordoba, Andalucia, Spain; 3Saint Peter's University Hospital/Robert Wood Johnson, New Brunswick, NJ; 4Saint Peter’s University Hospital, New Brunswick, NJ; 5Saint Peter's University Hospital/Robert Wood Johnson Hospital, New Brunswick, NJ; 6Orlando Gastroenterology PA, Orlando, FL
Introduction: Sessile serrated polyps, precursors to about one-third of colorectal cancers, are often missed due to their indistinct borders compared to tubular adenomas. The Serrated Polyp Detection Rate (SDR) is around 5.1% and is increasingly recognized as a key quality indicator for colonoscopy.
While many studies focus on adenoma detection rates by the training year of gastrointestinal fellows, research on detecting sessile serrated lesions during a three-year fellowship is limited. Our objective was to compare the detection rates of sessile serrated lesions (SDR) and conventional adenomas (ADR) across different stages of gastroenterology training.
Methods: We reviewed 1,603 screening colonoscopies (median age 57; 59.4% women) at our institute. Fourteen GI fellows performed 1,025 colonoscopies (63.9%): 201 (12.5%) by first years (F1s), 387 (24.1%) by second years (F2s), and 428 (26.7%) by third years (F3s).
Results: The overall SDR was 4.0%, and ADR was 46% in colonoscopies performed by attending physicians with fellows.
When comparing different years of training (Table 1), no significant differences in SDR were found among F1s, F2s, and F3s (3.5% vs. 4.1% vs. 5.6%, p=0.419). However, ADR was higher in F2s compared to F1s (50.9% vs. 42.3%, p=0.036) and in F3s compared to F1s (42.8% vs. 42.3%, p=0.036). There were no differences in the overall polyp detection rate (tubular adenoma, sessile serrated, and hyper-plastic polyps).
When comparing polyp detection rates by months of training (every six months and beyond), no significant differences were noted in ADR (46.0 vs. 39.2 vs. 50.0 vs. 50.6 vs. 42.3 vs. 44.5, p=0.276) or overall polyp detection rate (63.9 vs. 65.0 vs. 72.2 vs. 72.1 vs. 69.0 vs. 69.9, p=0.590), Figure 1. Similarly, no differences were noted in SDR between different months of training (4.0% vs. 2.9% vs. 3.6% vs. 6.0% vs. 5.0% vs. 6.1%, p=0.730).
Discussion: Our ADR exceeded the national benchmark, but our SDR fell below the recommended quality standard. The overall polyp detection rates and SDR do not show significant variations by year or months of training. Although there is some improvement in specific skills with experience (as seen with ADR in F2s), the overall detection abilities for polyps and sessile serrated remain relatively stable throughout the training period. It may be attributed to the challenges in detecting these lesions, even for board-certified endoscopists. It is imperative that training during fellowship should emphasize correctly detecting serrated lesions.
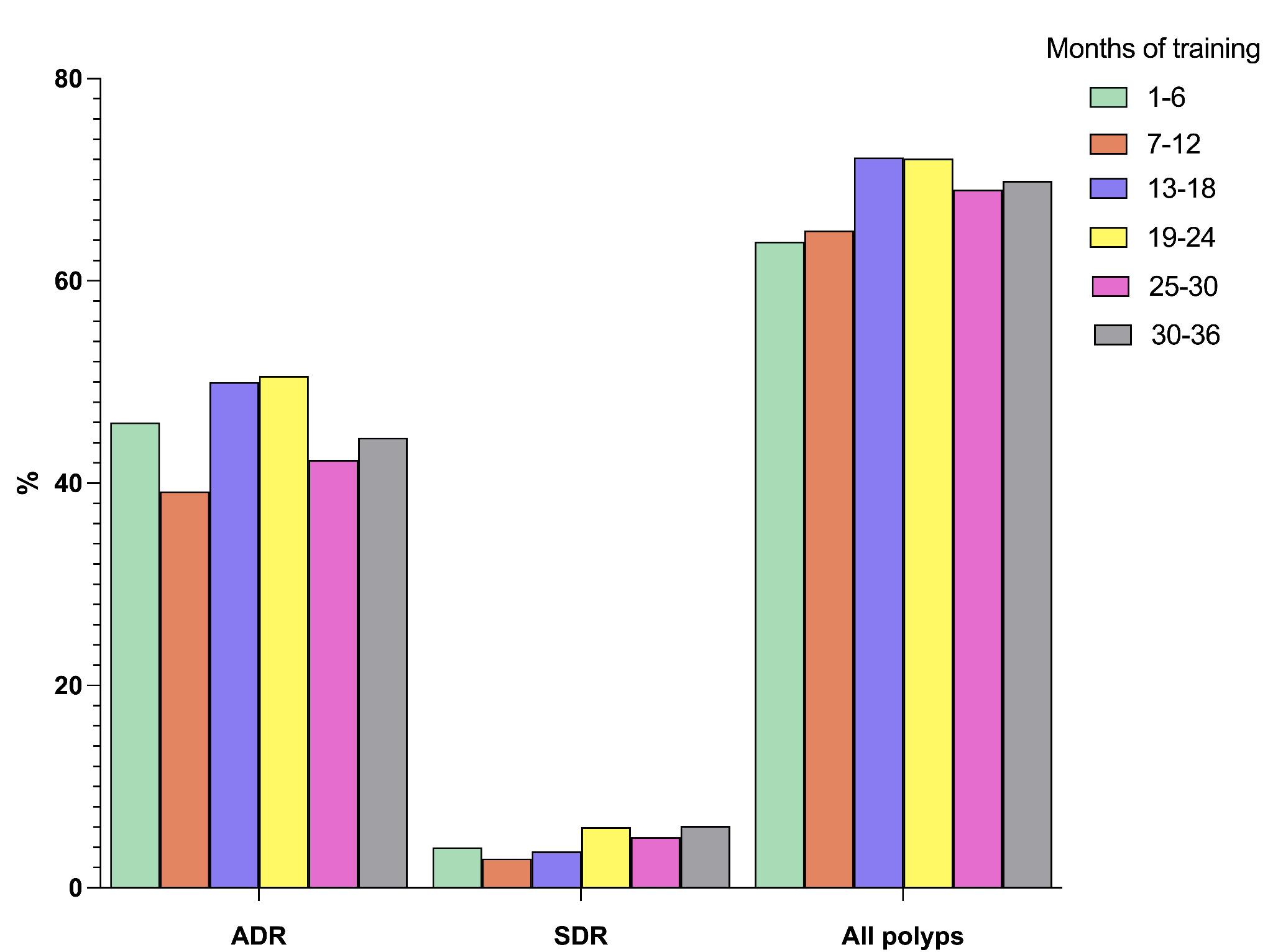
Figure: Figure 1: SDR, ADR, and total polyps by months of fellowship training
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mehak Bassi indicated no relevant financial relationships.
Archit Garg indicated no relevant financial relationships.
Beatriz Gros Alcade indicated no relevant financial relationships.
Aadhithyaraman Santharaman indicated no relevant financial relationships.
Khyati Bidani indicated no relevant financial relationships.
Richa Rani indicated no relevant financial relationships.
Mannat Kaur Bhatia indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Arkady Broder indicated no relevant financial relationships.
Mehak Bassi, MD1, Archit Garg, MD1, Beatriz Gros Alcade, MD2, Aadhithyaraman Santharaman, MD3, Khyati Bidani, MD4, Richa Rani, MD4, Mannat Kaur Bhatia, MD5, Babu Mohan, MD6, Arkady Broder, MD1. P4084 - The Link Between Trainee Participation in Colonoscopy Procedures and Quality Metrics, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

