Tuesday Poster Session
Category: General Endoscopy
P4106 - Iron Deficiency Anemia vs Iron Deficiency Without Anemia: A Difference in Endoscopic Management?
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- BA
Binyamin R. Abramowitz, MD
SUNY Downstate Health Sciences University
New York, NY
Presenting Author(s)
Binyamin R. Abramowitz, MD1, Sonny Caceres, MD2, Promila Banerjee, MD, FACG3, Ayse Aytaman, MD, FACG4, Daniel A. DiLeo, MD4, Bani Chander-Roland, MD, FACG5
1SUNY Downstate Health Sciences University, New York, NY; 2SUNY Downstate Medical Center, Brooklyn, NY; 3Edward Hines Jr. Veterans Affairs Hospital, Loyola University Chicago Stritch School of Medicine, Maywood, IL; 4Brooklyn VA Medical Center, Brooklyn, NY; 5VA NY Harbor Health System Clinical Associate Professor SUNY Downstate Health Sciences University, Brooklyn, NY
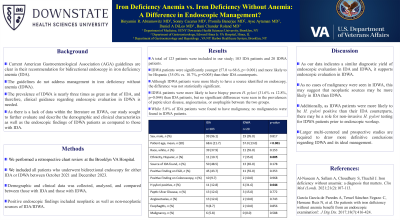
Introduction: Although current American Gastroenterological Association (AGA) guidelines are clear in their recommendation for bidirectional endoscopy in iron deficiency anemia (IDA), they do not address management in iron deficiency without anemia (IDWA). The prevalence of IDWA is nearly three times as great as that of IDA, and therefore, clinical guidance regarding endoscopic evaluation in IDWA is needed. As there is a lack of data within the literature on IDWA, our study sought to further evaluate and describe the demographic and clinical characteristics as well as the endoscopic findings of IDWA patients as compared to those with IDA.
Methods: We performed a retrospective chart review including all patients who underwent bidirectional endoscopy for either IDA or IDWA between October 2021 and December 2023 at the Brooklyn Campus of the VA New York Harbor Healthcare System. Demographic and clinical data was collected, analyzed, and compared between those with IDA and those with IDWA. Positive endoscopic findings included neoplastic as well as non-neoplastic sources of IDA/IDWA.
Results: A total of 123 patients were included in our study; 103 IDA patients and 20 IDWA patients. IDWA patients were significantly younger (57.0 vs 68.6, p< 0.001) and more likely to be Hispanic (35.0% vs. 10.7%, p=0.005) than their IDA counterparts. Although IDWA patients were more likely to have a source identified on endoscopy, the difference was not statistically significant. IDWA patients were more likely to have biopsy proven H. pylori (31.6% vs 12.8%, p=0.044) than IDA patients, but no significant differences were seen in the prevalences of peptic ulcer disease, angioectasias, or esophagitis between the two groups. While 5.8% of IDA patients were found to have malignancy, no malignancies were found in IDWA patients.
Discussion: As our data indicates a similar diagnostic yield of endoscopic evaluation in IDA and IDWA, it supports endoscopic evaluation in IDWA. As no cases of malignancy were seen in IDWA, this may suggest that neoplastic sources may be more likely in IDA than IDWA. Additionally, as IDWA patients were more likely to be H. pylori positive than their IDA counterparts, there may be a role for non-invasive H. pylori testing for IDWA patients prior to endoscopic workup. Larger multi-centered and prospective studies are required to draw more definitive conclusions regarding IDWA and its ideal management.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Binyamin R. Abramowitz, MD1, Sonny Caceres, MD2, Promila Banerjee, MD, FACG3, Ayse Aytaman, MD, FACG4, Daniel A. DiLeo, MD4, Bani Chander-Roland, MD, FACG5. P4106 - Iron Deficiency Anemia vs Iron Deficiency Without Anemia: A Difference in Endoscopic Management?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1SUNY Downstate Health Sciences University, New York, NY; 2SUNY Downstate Medical Center, Brooklyn, NY; 3Edward Hines Jr. Veterans Affairs Hospital, Loyola University Chicago Stritch School of Medicine, Maywood, IL; 4Brooklyn VA Medical Center, Brooklyn, NY; 5VA NY Harbor Health System Clinical Associate Professor SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Although current American Gastroenterological Association (AGA) guidelines are clear in their recommendation for bidirectional endoscopy in iron deficiency anemia (IDA), they do not address management in iron deficiency without anemia (IDWA). The prevalence of IDWA is nearly three times as great as that of IDA, and therefore, clinical guidance regarding endoscopic evaluation in IDWA is needed. As there is a lack of data within the literature on IDWA, our study sought to further evaluate and describe the demographic and clinical characteristics as well as the endoscopic findings of IDWA patients as compared to those with IDA.
Methods: We performed a retrospective chart review including all patients who underwent bidirectional endoscopy for either IDA or IDWA between October 2021 and December 2023 at the Brooklyn Campus of the VA New York Harbor Healthcare System. Demographic and clinical data was collected, analyzed, and compared between those with IDA and those with IDWA. Positive endoscopic findings included neoplastic as well as non-neoplastic sources of IDA/IDWA.
Results: A total of 123 patients were included in our study; 103 IDA patients and 20 IDWA patients. IDWA patients were significantly younger (57.0 vs 68.6, p< 0.001) and more likely to be Hispanic (35.0% vs. 10.7%, p=0.005) than their IDA counterparts. Although IDWA patients were more likely to have a source identified on endoscopy, the difference was not statistically significant. IDWA patients were more likely to have biopsy proven H. pylori (31.6% vs 12.8%, p=0.044) than IDA patients, but no significant differences were seen in the prevalences of peptic ulcer disease, angioectasias, or esophagitis between the two groups. While 5.8% of IDA patients were found to have malignancy, no malignancies were found in IDWA patients.
Discussion: As our data indicates a similar diagnostic yield of endoscopic evaluation in IDA and IDWA, it supports endoscopic evaluation in IDWA. As no cases of malignancy were seen in IDWA, this may suggest that neoplastic sources may be more likely in IDA than IDWA. Additionally, as IDWA patients were more likely to be H. pylori positive than their IDA counterparts, there may be a role for non-invasive H. pylori testing for IDWA patients prior to endoscopic workup. Larger multi-centered and prospective studies are required to draw more definitive conclusions regarding IDWA and its ideal management.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Binyamin Abramowitz indicated no relevant financial relationships.
Sonny Caceres indicated no relevant financial relationships.
Promila Banerjee indicated no relevant financial relationships.
Ayse Aytaman indicated no relevant financial relationships.
Daniel DiLeo indicated no relevant financial relationships.
Bani Chander-Roland indicated no relevant financial relationships.
Binyamin R. Abramowitz, MD1, Sonny Caceres, MD2, Promila Banerjee, MD, FACG3, Ayse Aytaman, MD, FACG4, Daniel A. DiLeo, MD4, Bani Chander-Roland, MD, FACG5. P4106 - Iron Deficiency Anemia vs Iron Deficiency Without Anemia: A Difference in Endoscopic Management?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

