Tuesday Poster Session
Category: General Endoscopy
P4107 - The Impact of Glycemic Control on Bowel Preparation Quality in Diabetic Patients
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- BA
Binyamin R. Abramowitz, MD
SUNY Downstate Health Sciences University
New York, NY
Presenting Author(s)
Binyamin R. Abramowitz, MD1, Gemechu S. Ayana, MD2, Promila Banerjee, MD, FACG3, Daniel A. DiLeo, MD4, Bani Chander-Roland, MD, FACG5
1SUNY Downstate Health Sciences University, New York, NY; 2SUNY Downstate Health Sciences University, Brooklyn, NY; 3Edward Hines Jr. Veterans Affairs Hospital, Loyola University Chicago Stritch School of Medicine, Maywood, IL; 4Brooklyn VA Medical Center, Brooklyn, NY; 5VA NY Harbor Health System Clinical Associate Professor SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: It is well-established that diabetes mellitus is associated with poor bowel preparation for colonoscopy. However, the impact of glycemic control on colonoscopy quality within diabetic patients has not been well defined. Minimal existing data has been contradictory; some studies have shown glycemic control to be associated with a higher adenoma detection rate, while other studies suggest that glycemic control does not influence the quality of bowel preparation. As the role of glycemic control in bowel preparation quality is not well defined, our study sought to determine whether optimization of glycemic control is associated with improved bowel preparation in diabetic patients.
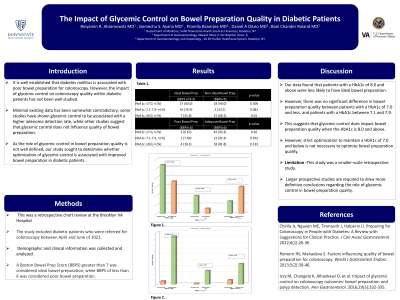
Methods: We performed a retrospective chart review including diabetic patients who were referred for colonoscopy at the New York Harbor Brooklyn VA Hospital Center between April and June of 2021. Demographic and clinical information was collected and analyzed. A Boston Bowel Prep Score (BBPS) greater than 7 was considered ideal bowel preparation, while BBPS of less than 6 was considered poor bowel preparation.
Results: A total of 80 patients were included in our study. The mean age was 66.5 years with black patients comprising 56.3% and Hispanic patients comprising 22.5% of the study cohort. 60.0% of those with a hemoglobin A1c (HbA1c) of 7.0 and below as well as 76.9% of those with a HbA1c between 7.1 and 7.9 were found to have ideal BBPS. In contrast, only 31.8% of patients with a HbA1c of 8.0 and above were found to be with ideal BBPS (p=0.010). Furthermore, 18.2% of those with a HbA1c of 8.0 and above were found to be with poor BBPS compared to 7.69% of those with a HbA1c between 7.1 and 7.9, and 6.67% of those with a HbA1c of 7.0 and below. These differences were not found to be statistically significant.
Discussion: Our data found that patients with a HbA1c of 8.0 and above were less likely to have ideal bowel preparation. However, there was no statistically significant difference in bowel preparation quality between patients with a HbA1c of 7.0 and less, and patients with a HbA1c between 7.1 and 7.9. This suggests that glycemic control does impact bowel preparation quality when the HbA1c is 8.0 and above. However, strict optimization to maintain a HbA1c of 7.0 and below is not necessary to optimize bowel preparation quality. As this study was a smaller-scale retrospective study, larger prospective studies are needed to better delineate the role of glycemic control in bowel preparation quality.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Binyamin R. Abramowitz, MD1, Gemechu S. Ayana, MD2, Promila Banerjee, MD, FACG3, Daniel A. DiLeo, MD4, Bani Chander-Roland, MD, FACG5. P4107 - The Impact of Glycemic Control on Bowel Preparation Quality in Diabetic Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1SUNY Downstate Health Sciences University, New York, NY; 2SUNY Downstate Health Sciences University, Brooklyn, NY; 3Edward Hines Jr. Veterans Affairs Hospital, Loyola University Chicago Stritch School of Medicine, Maywood, IL; 4Brooklyn VA Medical Center, Brooklyn, NY; 5VA NY Harbor Health System Clinical Associate Professor SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: It is well-established that diabetes mellitus is associated with poor bowel preparation for colonoscopy. However, the impact of glycemic control on colonoscopy quality within diabetic patients has not been well defined. Minimal existing data has been contradictory; some studies have shown glycemic control to be associated with a higher adenoma detection rate, while other studies suggest that glycemic control does not influence the quality of bowel preparation. As the role of glycemic control in bowel preparation quality is not well defined, our study sought to determine whether optimization of glycemic control is associated with improved bowel preparation in diabetic patients.
Methods: We performed a retrospective chart review including diabetic patients who were referred for colonoscopy at the New York Harbor Brooklyn VA Hospital Center between April and June of 2021. Demographic and clinical information was collected and analyzed. A Boston Bowel Prep Score (BBPS) greater than 7 was considered ideal bowel preparation, while BBPS of less than 6 was considered poor bowel preparation.
Results: A total of 80 patients were included in our study. The mean age was 66.5 years with black patients comprising 56.3% and Hispanic patients comprising 22.5% of the study cohort. 60.0% of those with a hemoglobin A1c (HbA1c) of 7.0 and below as well as 76.9% of those with a HbA1c between 7.1 and 7.9 were found to have ideal BBPS. In contrast, only 31.8% of patients with a HbA1c of 8.0 and above were found to be with ideal BBPS (p=0.010). Furthermore, 18.2% of those with a HbA1c of 8.0 and above were found to be with poor BBPS compared to 7.69% of those with a HbA1c between 7.1 and 7.9, and 6.67% of those with a HbA1c of 7.0 and below. These differences were not found to be statistically significant.
Discussion: Our data found that patients with a HbA1c of 8.0 and above were less likely to have ideal bowel preparation. However, there was no statistically significant difference in bowel preparation quality between patients with a HbA1c of 7.0 and less, and patients with a HbA1c between 7.1 and 7.9. This suggests that glycemic control does impact bowel preparation quality when the HbA1c is 8.0 and above. However, strict optimization to maintain a HbA1c of 7.0 and below is not necessary to optimize bowel preparation quality. As this study was a smaller-scale retrospective study, larger prospective studies are needed to better delineate the role of glycemic control in bowel preparation quality.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Binyamin Abramowitz indicated no relevant financial relationships.
Gemechu Ayana indicated no relevant financial relationships.
Promila Banerjee indicated no relevant financial relationships.
Daniel DiLeo indicated no relevant financial relationships.
Bani Chander-Roland indicated no relevant financial relationships.
Binyamin R. Abramowitz, MD1, Gemechu S. Ayana, MD2, Promila Banerjee, MD, FACG3, Daniel A. DiLeo, MD4, Bani Chander-Roland, MD, FACG5. P4107 - The Impact of Glycemic Control on Bowel Preparation Quality in Diabetic Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
