Tuesday Poster Session
Category: General Endoscopy
P4110 - Evaluating the Impact of Irritable Bowel Syndrome on Clinical Outcomes in Lower Gastrointestinal Bleeding
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- BA
Binyamin R. Abramowitz, MD
SUNY Downstate Health Sciences University
New York, NY
Presenting Author(s)
Binyamin R. Abramowitz, MD1, Viknesh Baskar, MD2, Alexander Kaye, MD3, Gemechu S. Ayana, MD2, Rachel R. Meier, BA4, Sushil Ahlawat, MD, MS, MBBS2
1SUNY Downstate Health Sciences University, New York, NY; 2SUNY Downstate Health Sciences University, Brooklyn, NY; 3SUNY Downstate Medical Center, Staten Island, NY; 4Columbia University, New York, NY
Introduction: Irritable bowel syndrome (IBS) is known to be an independent risk factor for poor outcomes in patients with other diseases such as Inflammatory Bowel Disease. The impact of IBS on clinical outcomes in lower gastrointestinal bleeding (LGIB) is relatively unknown as there are very few studies on the topic within the literature. We sought to evaluate outcomes of IBS patients hospitalized with LGIB in an effort to identify and delineate a potential relationship between IBS and LGIB.
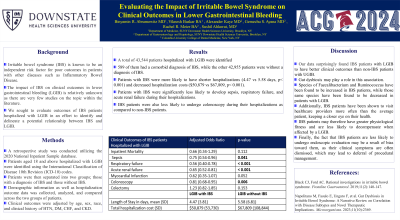
Methods: A retrospective study was conducted utilizing the 2020 National Inpatient Sample database. Patients aged 18 and above hospitalized with LGIB were identified using the International Classification of Disease 10th Revision (ICD-10) codes. Patients were then separated into two groups; those with a diagnosis of IBS and those without IBS. Demographic information as well as hospitalization outcome data was collected, analyzed, and compared across the two groups of patients. Clinical outcomes were adjusted by age, sex, race, and clinical history of HTN, DM, CHF, and CKD.
Results: A total of 43,544 patients hospitalized with LGIB were identified; 589 of them had a comorbid diagnosis of IBS, while the other 42,955 patients were without a diagnosis of IBS. Patients with IBS were more likely to have shorter hospitalizations (4.47 vs 5.58 days, p< 0.001) and decreased hospitalization costs ($50,879 vs $67,809, p< 0.001). Patients with IBS were significantly less likely to develop sepsis, respiratory failure, and acute renal failure during their hospitalizations. IBS patients were also less likely to undergo colonoscopy during their hospitalizations as compared to non-IBS patients.
Discussion: Our data surprisingly found IBS patients with LGIB to have better clinical outcomes than non-IBS patients with UGIB. Gut dysbiosis may play a role in this association. Species of Faecalibacterium and Ruminococcus have been found to be increased in IBS patients, while those same species have been found to be decreased in patients with LGIB. Additionally, IBS patients have been shown to visit healthcare providers more often than the average patient, keeping a closer eye on their health. IBS patients may therefore have greater physiological fitness and are less likely to decompensate when affected by a LGIB. Finally, the fact that IBS patients are less likely to undergo endoscopic evaluation may be a result of bias toward them, as their clinical symptoms are often dismissed, which may lead to deferral of procedural management.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Binyamin R. Abramowitz, MD1, Viknesh Baskar, MD2, Alexander Kaye, MD3, Gemechu S. Ayana, MD2, Rachel R. Meier, BA4, Sushil Ahlawat, MD, MS, MBBS2. P4110 - Evaluating the Impact of Irritable Bowel Syndrome on Clinical Outcomes in Lower Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1SUNY Downstate Health Sciences University, New York, NY; 2SUNY Downstate Health Sciences University, Brooklyn, NY; 3SUNY Downstate Medical Center, Staten Island, NY; 4Columbia University, New York, NY
Introduction: Irritable bowel syndrome (IBS) is known to be an independent risk factor for poor outcomes in patients with other diseases such as Inflammatory Bowel Disease. The impact of IBS on clinical outcomes in lower gastrointestinal bleeding (LGIB) is relatively unknown as there are very few studies on the topic within the literature. We sought to evaluate outcomes of IBS patients hospitalized with LGIB in an effort to identify and delineate a potential relationship between IBS and LGIB.
Methods: A retrospective study was conducted utilizing the 2020 National Inpatient Sample database. Patients aged 18 and above hospitalized with LGIB were identified using the International Classification of Disease 10th Revision (ICD-10) codes. Patients were then separated into two groups; those with a diagnosis of IBS and those without IBS. Demographic information as well as hospitalization outcome data was collected, analyzed, and compared across the two groups of patients. Clinical outcomes were adjusted by age, sex, race, and clinical history of HTN, DM, CHF, and CKD.
Results: A total of 43,544 patients hospitalized with LGIB were identified; 589 of them had a comorbid diagnosis of IBS, while the other 42,955 patients were without a diagnosis of IBS. Patients with IBS were more likely to have shorter hospitalizations (4.47 vs 5.58 days, p< 0.001) and decreased hospitalization costs ($50,879 vs $67,809, p< 0.001). Patients with IBS were significantly less likely to develop sepsis, respiratory failure, and acute renal failure during their hospitalizations. IBS patients were also less likely to undergo colonoscopy during their hospitalizations as compared to non-IBS patients.
Discussion: Our data surprisingly found IBS patients with LGIB to have better clinical outcomes than non-IBS patients with UGIB. Gut dysbiosis may play a role in this association. Species of Faecalibacterium and Ruminococcus have been found to be increased in IBS patients, while those same species have been found to be decreased in patients with LGIB. Additionally, IBS patients have been shown to visit healthcare providers more often than the average patient, keeping a closer eye on their health. IBS patients may therefore have greater physiological fitness and are less likely to decompensate when affected by a LGIB. Finally, the fact that IBS patients are less likely to undergo endoscopic evaluation may be a result of bias toward them, as their clinical symptoms are often dismissed, which may lead to deferral of procedural management.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Binyamin Abramowitz indicated no relevant financial relationships.
Viknesh Baskar indicated no relevant financial relationships.
Alexander Kaye indicated no relevant financial relationships.
Gemechu Ayana indicated no relevant financial relationships.
Rachel Meier indicated no relevant financial relationships.
Sushil Ahlawat indicated no relevant financial relationships.
Binyamin R. Abramowitz, MD1, Viknesh Baskar, MD2, Alexander Kaye, MD3, Gemechu S. Ayana, MD2, Rachel R. Meier, BA4, Sushil Ahlawat, MD, MS, MBBS2. P4110 - Evaluating the Impact of Irritable Bowel Syndrome on Clinical Outcomes in Lower Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
