Tuesday Poster Session
Category: General Endoscopy
P4112 - Barriers to Endoscopy Completion in a Safety Net Hospital
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SC
Sindhu Chadalawada, MD
Alameda Health System
Fresno, CA
Presenting Author(s)
Sindhu Chadalawada, MD1, Simon Sabir, DO1, Thanh Ngoc. Nguyen, MD1, Kala Mehta, MPH2, Farzad Moazed, MD1, Christina Chou, MD1
1Alameda Health System, Oakland, CA; 2University of California San Francisco, San Francisco, CA
Introduction: Safety net systems nationwide serve marginalized populations. Healthcare delivery and efficiency in these resource limited settings are impeded by patient no shows and cancellations. Endoscopy suites are significantly affected by this and consequently, can lead to underutilization, increasing unit overhead and operating expenses. Downstream effects include delays in care, prolonged wait times, and adverse health outcomes. Approximately a third of scheduled patients at a safety net in Oakland do not complete their scheduled outpatient procedures. We aim to better understand the social determinants of health and barriers at play contributing to the lack of completion of procedures.
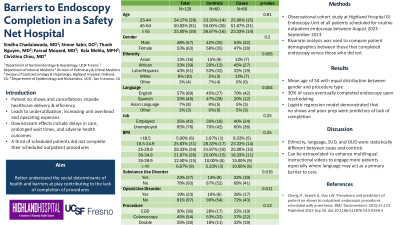
Methods: An observational cohort study was conducted at Highland Hospital GI Endoscopy Unit of all patients scheduled for routine outpatient endoscopy between August 2023 - September 2023. Duplicated patients were removed from the dataset. Bivariate analysis was used to compare patient demographics between those that completed endoscopy versus those who did not.
Results: 120 patients were enrolled in the cohort of which 60 patients completed endoscopy as scheduled. The mean age was 54 years with an equal distribution amongst gender and type of procedure (i.e. EGD, colonoscopy or double). Majority of patients were African American (45%) among cases and Latino (53%) among controls which was statistically significant (p-value 0.005). Cohort was composed primarily of English and Spanish speakers (p-value 0.004). 32% of cases were noted to have a substance use disorder compared to 13% among controls (p-value 0.016). 30% of cases eventually completed endoscopy upon rescheduling. A logistic regression model demonstrated that patient no shows and poor prep were predictors of lack of completion.
Discussion: Ethnicity, language, substance use disorder, and opioid use disorders were statistically different between cases and controls. Poor preparation also correlated to lack of endoscopy completion. Application of this data can be extrapolated to focusing on patient education through quality improvement measures to enhance educational tools such as multilingual instructional videos to engage more patients especially where language may act as a primary barrier to care.
Disclosures:
Sindhu Chadalawada, MD1, Simon Sabir, DO1, Thanh Ngoc. Nguyen, MD1, Kala Mehta, MPH2, Farzad Moazed, MD1, Christina Chou, MD1. P4112 - Barriers to Endoscopy Completion in a Safety Net Hospital, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Alameda Health System, Oakland, CA; 2University of California San Francisco, San Francisco, CA
Introduction: Safety net systems nationwide serve marginalized populations. Healthcare delivery and efficiency in these resource limited settings are impeded by patient no shows and cancellations. Endoscopy suites are significantly affected by this and consequently, can lead to underutilization, increasing unit overhead and operating expenses. Downstream effects include delays in care, prolonged wait times, and adverse health outcomes. Approximately a third of scheduled patients at a safety net in Oakland do not complete their scheduled outpatient procedures. We aim to better understand the social determinants of health and barriers at play contributing to the lack of completion of procedures.
Methods: An observational cohort study was conducted at Highland Hospital GI Endoscopy Unit of all patients scheduled for routine outpatient endoscopy between August 2023 - September 2023. Duplicated patients were removed from the dataset. Bivariate analysis was used to compare patient demographics between those that completed endoscopy versus those who did not.
Results: 120 patients were enrolled in the cohort of which 60 patients completed endoscopy as scheduled. The mean age was 54 years with an equal distribution amongst gender and type of procedure (i.e. EGD, colonoscopy or double). Majority of patients were African American (45%) among cases and Latino (53%) among controls which was statistically significant (p-value 0.005). Cohort was composed primarily of English and Spanish speakers (p-value 0.004). 32% of cases were noted to have a substance use disorder compared to 13% among controls (p-value 0.016). 30% of cases eventually completed endoscopy upon rescheduling. A logistic regression model demonstrated that patient no shows and poor prep were predictors of lack of completion.
Discussion: Ethnicity, language, substance use disorder, and opioid use disorders were statistically different between cases and controls. Poor preparation also correlated to lack of endoscopy completion. Application of this data can be extrapolated to focusing on patient education through quality improvement measures to enhance educational tools such as multilingual instructional videos to engage more patients especially where language may act as a primary barrier to care.
Disclosures:
Sindhu Chadalawada indicated no relevant financial relationships.
Simon Sabir indicated no relevant financial relationships.
Thanh Nguyen indicated no relevant financial relationships.
Kala Mehta indicated no relevant financial relationships.
Farzad Moazed indicated no relevant financial relationships.
Christina Chou indicated no relevant financial relationships.
Sindhu Chadalawada, MD1, Simon Sabir, DO1, Thanh Ngoc. Nguyen, MD1, Kala Mehta, MPH2, Farzad Moazed, MD1, Christina Chou, MD1. P4112 - Barriers to Endoscopy Completion in a Safety Net Hospital, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
