Tuesday Poster Session
Category: General Endoscopy
P4126 - Gastrojejunocolic Fistula Formation After EUS-GJ
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MS
Michael Saadeh, MD
University Hospitals Cleveland Medical Center, Case Western Reserve University
Cleveland, OH
Presenting Author(s)
Michael Saadeh, MD1, Sofi Damjanovska, MD1, Apoorva K. Chandar, MBBS, MPH2, Vibhu Chittajallu, MD3, Brooke Glessing, MD4, Andrew Catanzaro, MD4
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2Case Western Reserve University School of Medicine, Cleveland, OH; 3West Virginia University, Cleveland, OH; 4Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Endoscopic ultrasound-guided gastrojejunostomy (EUS-GJ) offers treatment for malignant gastric outlet obstruction. The procedure provides an alternative for those with a terminal illness and/or contraindications for surgery or enteral stent placement. Studies comparing the three treatment options have shown a decreased risk of reintervention and adverse events after EUS-GJ. Adverse events related to EUS-GJ include abdominal pain, peritonitis, bleeding, and, rarely, stent misdeployment.
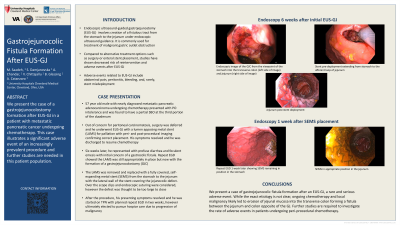
Case Description/Methods: A 57 year old male with newly diagnosed metastatic pancreatic adenocarcinoma undergoing chemotherapy presented with partial small bowel obstruction at the third portion of the duodenum with per oral intolerance. He was deemed not a surgical candidate due to new concern of peritoneal carcinomatosis and instead underwent EUS-GJ with a lumen apposing metal stent (LAMS) for palliation with intra- and post-procedural imaging confirming correct placement. There was no suggestion of interposing colon or bowel damage. His symptoms resolved and he was discharged to resume chemotherapy. Six weeks later, he represented after developing profuse diarrhea and feculent emesis with concern of a gastrocolic fistula. Repeat EGD showed the LAMS was still appropriately in place but now with the formation of a gastrojejunocolic fistula (GJF). It was thought the GJF formation was a result of inflammation from his malignancy and chemotherapy, leading to erosion of jejunal mucosa into the transverse colon forming a fistula between the jejunum and colon opposite the GJ. The LAMS was removed and replaced with a fully covered, self-expanding metal stent from the stomach to the jejunum with the lateral wall of the stent covering the jejunocolic defect. Over the scope clips and endoscopic suturing were considered, however the defect was thought to be too large to close. After the procedure, his presenting symptoms resolved and he was started on TPN with planned repeat EGD in two weeks, however ultimately elected to pursue hospice care due to progression of metastatic malignancy.
Discussion: We present a rare and severe adverse event after EUS-GJ. While the exact etiology is not clear, ongoing chemotherapy and locally invasive malignancy likely played a significant role in the development of the GJF. Further studies are required to investigate the rate of adverse events in patients undergoing peri-procedural chemotherapy.
Disclosures:
Michael Saadeh, MD1, Sofi Damjanovska, MD1, Apoorva K. Chandar, MBBS, MPH2, Vibhu Chittajallu, MD3, Brooke Glessing, MD4, Andrew Catanzaro, MD4. P4126 - Gastrojejunocolic Fistula Formation After EUS-GJ, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 2Case Western Reserve University School of Medicine, Cleveland, OH; 3West Virginia University, Cleveland, OH; 4Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Endoscopic ultrasound-guided gastrojejunostomy (EUS-GJ) offers treatment for malignant gastric outlet obstruction. The procedure provides an alternative for those with a terminal illness and/or contraindications for surgery or enteral stent placement. Studies comparing the three treatment options have shown a decreased risk of reintervention and adverse events after EUS-GJ. Adverse events related to EUS-GJ include abdominal pain, peritonitis, bleeding, and, rarely, stent misdeployment.
Case Description/Methods: A 57 year old male with newly diagnosed metastatic pancreatic adenocarcinoma undergoing chemotherapy presented with partial small bowel obstruction at the third portion of the duodenum with per oral intolerance. He was deemed not a surgical candidate due to new concern of peritoneal carcinomatosis and instead underwent EUS-GJ with a lumen apposing metal stent (LAMS) for palliation with intra- and post-procedural imaging confirming correct placement. There was no suggestion of interposing colon or bowel damage. His symptoms resolved and he was discharged to resume chemotherapy. Six weeks later, he represented after developing profuse diarrhea and feculent emesis with concern of a gastrocolic fistula. Repeat EGD showed the LAMS was still appropriately in place but now with the formation of a gastrojejunocolic fistula (GJF). It was thought the GJF formation was a result of inflammation from his malignancy and chemotherapy, leading to erosion of jejunal mucosa into the transverse colon forming a fistula between the jejunum and colon opposite the GJ. The LAMS was removed and replaced with a fully covered, self-expanding metal stent from the stomach to the jejunum with the lateral wall of the stent covering the jejunocolic defect. Over the scope clips and endoscopic suturing were considered, however the defect was thought to be too large to close. After the procedure, his presenting symptoms resolved and he was started on TPN with planned repeat EGD in two weeks, however ultimately elected to pursue hospice care due to progression of metastatic malignancy.
Discussion: We present a rare and severe adverse event after EUS-GJ. While the exact etiology is not clear, ongoing chemotherapy and locally invasive malignancy likely played a significant role in the development of the GJF. Further studies are required to investigate the rate of adverse events in patients undergoing peri-procedural chemotherapy.
Disclosures:
Michael Saadeh indicated no relevant financial relationships.
Sofi Damjanovska indicated no relevant financial relationships.
Apoorva Chandar indicated no relevant financial relationships.
Vibhu Chittajallu indicated no relevant financial relationships.
Brooke Glessing indicated no relevant financial relationships.
Andrew Catanzaro indicated no relevant financial relationships.
Michael Saadeh, MD1, Sofi Damjanovska, MD1, Apoorva K. Chandar, MBBS, MPH2, Vibhu Chittajallu, MD3, Brooke Glessing, MD4, Andrew Catanzaro, MD4. P4126 - Gastrojejunocolic Fistula Formation After EUS-GJ, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
