Tuesday Poster Session
Category: GI Bleeding
P4167 - Management and Outcomes of Gastric Varices: A Retrospective Study
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Reece Wadle, MD
Mayo Clinic School of Graduate Medical Education
Rochester, MN
Presenting Author(s)
Award: Presidential Poster Award
Reece Wadle, MD1, Louma Basma O. Rustam, MD2, Antonio J. Sanchez, MD3
1Mayo Clinic School of Graduate Medical Education, Rochester, MN; 2University of Iowa Hospitals and Clinics, Iowa City, IA; 3University of Iowa Hospitals & Clinics, Iowa City, IA
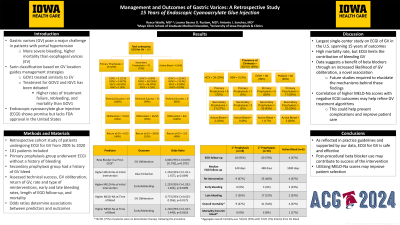
Introduction: Gastric varices (GV) pose a major challenge in patients with portal hypertension due to their propensity for severe bleeding and higher mortality when compared to esophageal varices (EV). The Sarin classification is based on GV location and guides management strategies. While GOV1 can be treated similarly to EV, optimal management for GOV2 and IGV1 has been debated due to higher rates of treatment failure, rebleeding, and mortality. Endoscopic cyanoacrylate glue injection (ECGI) shows promise but lacks FDA approval in the United States.
Methods: We used the TriNetX platform to perform a retrospective cohort study of patients who underwent ECGI for GV from 2005 to 2020. Charts of 101 patients were reviewed. Assessed outcomes included technical success, GV obliteration, return of GV, rate and type of reinterventions, early and late rebleeding rates, length of EGD follow-up, and mortality. Odds ratios were calculated to determine significant associations between predictors and outcomes.
Results: 76/101 (75%) of patients were on beta blockers following gluing, which was associated with an increased likelihood of GV obliteration (OR=4.846 [95% CI=0.878-26.742], p=0.0701). A Higher MELD-Na score at the time of initial intervention was associated with a higher risk of glue embolism (OR=1.254 [95% CI=1.011-1.557], p=0.0396) and early rebleeding (OR=1.229 [95% CI=1.032-1.465], p=0.0209). Higher MELD-Na score at the time of a bleed was associated with a decreased likelihood of GV obliteration (OR=0.773 [95% CI=0.625-0.956], p=0.0175) and increased likelihood of early rebleeding (OR=1.210 [95% CI=1.017-1.440], p=0.0318). Mortality rates during the follow-up period were high (54/101=53.5%), but few deaths were directly attributable to GV bleeding (7/101=6.9%).
Discussion: To our knowledge, this is the largest single-center study on the management and long-term outcomes of GV in the U.S. As reflected in practice guidelines and supported by our data, ECGI for GV is safe and effective. While mortality rates are high in this population, ECGI limits the contribution of bleeding GV. Our data suggests a benefit of beta blockers through an increased likelihood of GV obliteration, a novel association. Future studies are required to elucidate the mechanisms behind these findings. Exploring the correlation of higher MELD-Na scores with negative ECGI outcomes may help refine GV treatment algorithms, prevent complications, and improve patient care.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Reece Wadle, MD1, Louma Basma O. Rustam, MD2, Antonio J. Sanchez, MD3. P4167 - Management and Outcomes of Gastric Varices: A Retrospective Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Reece Wadle, MD1, Louma Basma O. Rustam, MD2, Antonio J. Sanchez, MD3
1Mayo Clinic School of Graduate Medical Education, Rochester, MN; 2University of Iowa Hospitals and Clinics, Iowa City, IA; 3University of Iowa Hospitals & Clinics, Iowa City, IA
Introduction: Gastric varices (GV) pose a major challenge in patients with portal hypertension due to their propensity for severe bleeding and higher mortality when compared to esophageal varices (EV). The Sarin classification is based on GV location and guides management strategies. While GOV1 can be treated similarly to EV, optimal management for GOV2 and IGV1 has been debated due to higher rates of treatment failure, rebleeding, and mortality. Endoscopic cyanoacrylate glue injection (ECGI) shows promise but lacks FDA approval in the United States.
Methods: We used the TriNetX platform to perform a retrospective cohort study of patients who underwent ECGI for GV from 2005 to 2020. Charts of 101 patients were reviewed. Assessed outcomes included technical success, GV obliteration, return of GV, rate and type of reinterventions, early and late rebleeding rates, length of EGD follow-up, and mortality. Odds ratios were calculated to determine significant associations between predictors and outcomes.
Results: 76/101 (75%) of patients were on beta blockers following gluing, which was associated with an increased likelihood of GV obliteration (OR=4.846 [95% CI=0.878-26.742], p=0.0701). A Higher MELD-Na score at the time of initial intervention was associated with a higher risk of glue embolism (OR=1.254 [95% CI=1.011-1.557], p=0.0396) and early rebleeding (OR=1.229 [95% CI=1.032-1.465], p=0.0209). Higher MELD-Na score at the time of a bleed was associated with a decreased likelihood of GV obliteration (OR=0.773 [95% CI=0.625-0.956], p=0.0175) and increased likelihood of early rebleeding (OR=1.210 [95% CI=1.017-1.440], p=0.0318). Mortality rates during the follow-up period were high (54/101=53.5%), but few deaths were directly attributable to GV bleeding (7/101=6.9%).
Discussion: To our knowledge, this is the largest single-center study on the management and long-term outcomes of GV in the U.S. As reflected in practice guidelines and supported by our data, ECGI for GV is safe and effective. While mortality rates are high in this population, ECGI limits the contribution of bleeding GV. Our data suggests a benefit of beta blockers through an increased likelihood of GV obliteration, a novel association. Future studies are required to elucidate the mechanisms behind these findings. Exploring the correlation of higher MELD-Na scores with negative ECGI outcomes may help refine GV treatment algorithms, prevent complications, and improve patient care.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Reece Wadle indicated no relevant financial relationships.
Louma Basma Rustam indicated no relevant financial relationships.
Antonio Sanchez: Abbvie – Grant/Research Support. Boehringer-Ingelheim – Grant/Research Support. Gilead – Grant/Research Support. Inventiva – Grant/Research Support. Ipsen – Advisory Committee/Board Member. Merck – Grant/Research Support. Mirum Pharmaceuticals – Grant/Research Support. Takeda – Grant/Research Support.
Reece Wadle, MD1, Louma Basma O. Rustam, MD2, Antonio J. Sanchez, MD3. P4167 - Management and Outcomes of Gastric Varices: A Retrospective Study, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

