Tuesday Poster Session
Category: GI Bleeding
P4174 - Demographic Differences in Outcomes for Hospitalizations With Lower Gastrointestinal Bleeding in the United States
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- AD
Apoorva Doshi, MBBS
Seth Gordhandas Sundardas Medical College and KEM Hospital
Birmingham, AL
Presenting Author(s)
Apoorva Doshi, MBBS1, Devina Adlaja, MD2, Lefika Bathobakae, MD3, Rashmi Advani, MD4, Kamal Amer, MD5
1Seth Gordhandas Sundardas Medical College and KEM Hospital, Birmingham, AL; 2St. Joseph’s University Medical Center, Paterson, NJ; 3St. Joseph's University Medical Center, Paterson, NJ; 4Icahn School of Medicine at Mount Sinai, New York, NY; 5St. Joseph's University Medical Center, Paterson, NJ
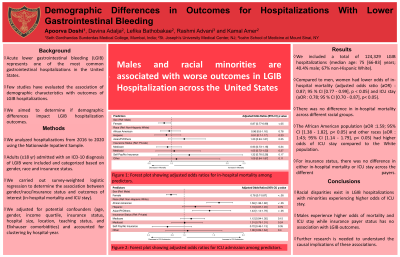
Introduction: Acute lower gastrointestinal bleeding (LGIB) represents one of the most common gastrointestinal hospitalizations in the United States. Few studies have evaluated the association of demographic characteristics with outcomes of LGIB hospitalizations. We aimed to determine if demographic differences impact LGIB hospitalization outcomes.
Methods: We analyzed hospitalizations from 2016 to 2020 using the Nationwide Inpatient Sample. Adults (≥18 yr) admitted with an ICD-10 diagnosis of LGIB were included and categorized based on gender, race and insurance status. We carried out survey-weighted logistic regression to determine the association between gender/race/insurance status and outcomes of interest (in-hospital mortality and ICU stay). We adjusted for potential confounders (age, gender, income quartile, insurance status, hospital size, location, teaching status, and Elixhauser comorbidities) and accounted for clustering by hospital-year.
Results: We included a total of 124,329 LGIB hospitalizations (median age: 75 [66-83] years). Of these, 50.6% were female, 67% were White, 19% were African American, 8% were Hispanic and 5% were other races. The insurance payer for a majority of hospitalizations was Medicare (76%), followed by Private insurance (14%) and Medicaid (6%). Compared to men, women had lower odds of in-hospital mortality (adjusted odds ratio (aOR) : 0.87; 95 % CI [0.77 - 0.99], p < 0.05) and ICU stay (aOR : 0.78; 95 % CI [0.70 - 0.87], p< 0.05). After multivariate adjustment, there was no difference in in-hospital mortality across different racial groups. However, the African American population (aOR :1.59; 95% CI [1.38 - 1.82], p< 0.05) and other races (aOR : 1:43; 95% CI [1.14 - 1.79], p< 0.05) had higher odds of ICU stay compared to the White population. For insurance status, there was no difference in either in-hospital mortality or ICU stay across the different payers.
Discussion: Gender differences exist in outcomes of LGIB hospitalizations with females experiencing lower odds of in-hospital mortality and ICU stay whereas racial differences only impact ICU stay with higher odds for African Americans and other races and no difference for Hispanics compared to White population. Additionally, the type of insurance had no impact on outcomes of interest. Further studies are required to understand specific risk factors contributing to the gender and racial disparities.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Apoorva Doshi, MBBS1, Devina Adlaja, MD2, Lefika Bathobakae, MD3, Rashmi Advani, MD4, Kamal Amer, MD5. P4174 - Demographic Differences in Outcomes for Hospitalizations With Lower Gastrointestinal Bleeding in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Seth Gordhandas Sundardas Medical College and KEM Hospital, Birmingham, AL; 2St. Joseph’s University Medical Center, Paterson, NJ; 3St. Joseph's University Medical Center, Paterson, NJ; 4Icahn School of Medicine at Mount Sinai, New York, NY; 5St. Joseph's University Medical Center, Paterson, NJ
Introduction: Acute lower gastrointestinal bleeding (LGIB) represents one of the most common gastrointestinal hospitalizations in the United States. Few studies have evaluated the association of demographic characteristics with outcomes of LGIB hospitalizations. We aimed to determine if demographic differences impact LGIB hospitalization outcomes.
Methods: We analyzed hospitalizations from 2016 to 2020 using the Nationwide Inpatient Sample. Adults (≥18 yr) admitted with an ICD-10 diagnosis of LGIB were included and categorized based on gender, race and insurance status. We carried out survey-weighted logistic regression to determine the association between gender/race/insurance status and outcomes of interest (in-hospital mortality and ICU stay). We adjusted for potential confounders (age, gender, income quartile, insurance status, hospital size, location, teaching status, and Elixhauser comorbidities) and accounted for clustering by hospital-year.
Results: We included a total of 124,329 LGIB hospitalizations (median age: 75 [66-83] years). Of these, 50.6% were female, 67% were White, 19% were African American, 8% were Hispanic and 5% were other races. The insurance payer for a majority of hospitalizations was Medicare (76%), followed by Private insurance (14%) and Medicaid (6%). Compared to men, women had lower odds of in-hospital mortality (adjusted odds ratio (aOR) : 0.87; 95 % CI [0.77 - 0.99], p < 0.05) and ICU stay (aOR : 0.78; 95 % CI [0.70 - 0.87], p< 0.05). After multivariate adjustment, there was no difference in in-hospital mortality across different racial groups. However, the African American population (aOR :1.59; 95% CI [1.38 - 1.82], p< 0.05) and other races (aOR : 1:43; 95% CI [1.14 - 1.79], p< 0.05) had higher odds of ICU stay compared to the White population. For insurance status, there was no difference in either in-hospital mortality or ICU stay across the different payers.
Discussion: Gender differences exist in outcomes of LGIB hospitalizations with females experiencing lower odds of in-hospital mortality and ICU stay whereas racial differences only impact ICU stay with higher odds for African Americans and other races and no difference for Hispanics compared to White population. Additionally, the type of insurance had no impact on outcomes of interest. Further studies are required to understand specific risk factors contributing to the gender and racial disparities.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Apoorva Doshi indicated no relevant financial relationships.
Devina Adlaja indicated no relevant financial relationships.
Lefika Bathobakae indicated no relevant financial relationships.
Rashmi Advani indicated no relevant financial relationships.
Kamal Amer indicated no relevant financial relationships.
Apoorva Doshi, MBBS1, Devina Adlaja, MD2, Lefika Bathobakae, MD3, Rashmi Advani, MD4, Kamal Amer, MD5. P4174 - Demographic Differences in Outcomes for Hospitalizations With Lower Gastrointestinal Bleeding in the United States, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
