Tuesday Poster Session
Category: GI Bleeding
P4181 - Racial Disparities in Patients With Non-Variceal Upper Gastrointestinal Bleeding in Patients According to a Large National Dataset
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio

M Kenan Rahima, MD
TriHealth Good Samaritan Hospital
Cincinnati, OH
Presenting Author(s)
M Kenan Rahima, MD1, Mohamad Hijazi, MD1, Mhd Kutaiba Albuni, MD2, Venkata Muddana, MD3
1TriHealth Good Samaritan Hospital, Cincinnati, OH; 2TriHealth, Doha, Ad Dawhah, Qatar; 3TriHealth, Cincinnati, OH
Introduction: Racial disparities in healthcare refer to differences in health outcomes, access to healthcare services, and quality of care among different racial or ethnic groups. Understanding these disparities is essential for improving healthcare equity and ensuring that all patients receive appropriate and equitable care regardless of their racial or ethnic background. The aim of this study was to investigate the basic characteristics and clinical outcomes of racial differences in patients admitted with NVUGIB.
Methods: We queried the National Inpatient Sample between 2017 and 2020 for adult patients of different races who were hospitalized with NVUGIB. The primary outcome was inpatient mortality. Multivariable logistic, linear, and Poisson regression analyses were used to estimate clinical outcomes with a p-value < 0.05 was significant.
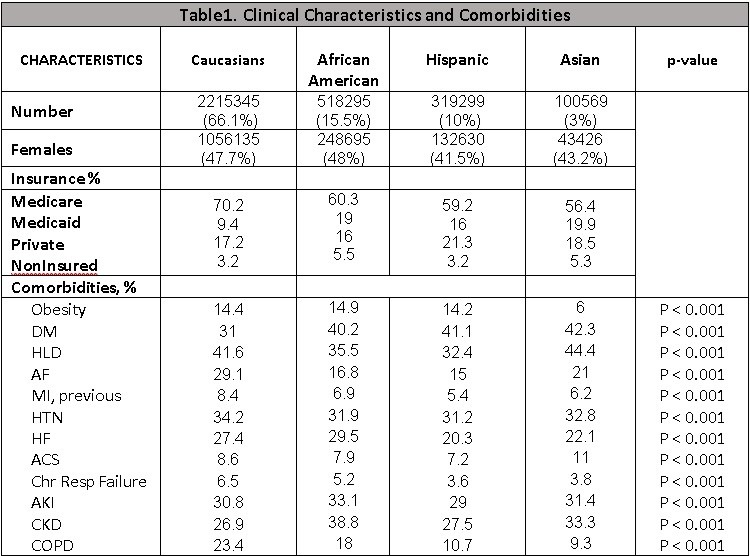
Results: There were 3,349,779 hospitalizations with NVUGIB. Mean age was 67 yrs and 53.2% were male. Among the admitted patients, Caucasians were 2,215,345 (66.1%), Blacks were 518,295 (15.5) and other races were 616,137 (18.4%). Subgroup with Caucasians, Blacks and other races had Medicare 70.1% vs 60.3% vs 54.9%, Medicaid 9.4% vs 18.9% vs 15.6%, obesity 14.4% vs 14.9% vs 11%, respectively. All-cause mortality in patients admitted with NVUGIB was 235,385, where subgroup with Caucasians, Blacks and other races had 149,860 (6.8%) vs 34,655 (6.7%) vs 50867 (8.6%). The racial subgroup showed significant primary and secondary outcomes that are presented in Table 1 with comorbidities in Table 2.
Discussion: All obtained results revealed statistical significance and we considered Caucasian population as baseline. Mortality, intensive care services and resource utilization proportion was highest among Asian race followed by Hispanic race then by Black race. Cardiac arrest proportion was highest among Black race followed by Asian race then by Hispanic race. LOS was highest among Asian race followed by Black race then by Hispanic race. Understanding these disparities is essential for improving healthcare equity and ensuring that all patients receive appropriate and equitable care regardless of their racial or ethnic background. Addressing these disparities might involve interventions such as improving access to healthcare services, and culturally competent care, and addressing social determinants of health that disproportionately affect certain racial or ethnic groups.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
M Kenan Rahima, MD1, Mohamad Hijazi, MD1, Mhd Kutaiba Albuni, MD2, Venkata Muddana, MD3. P4181 - Racial Disparities in Patients With Non-Variceal Upper Gastrointestinal Bleeding in Patients According to a Large National Dataset, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1TriHealth Good Samaritan Hospital, Cincinnati, OH; 2TriHealth, Doha, Ad Dawhah, Qatar; 3TriHealth, Cincinnati, OH
Introduction: Racial disparities in healthcare refer to differences in health outcomes, access to healthcare services, and quality of care among different racial or ethnic groups. Understanding these disparities is essential for improving healthcare equity and ensuring that all patients receive appropriate and equitable care regardless of their racial or ethnic background. The aim of this study was to investigate the basic characteristics and clinical outcomes of racial differences in patients admitted with NVUGIB.
Methods: We queried the National Inpatient Sample between 2017 and 2020 for adult patients of different races who were hospitalized with NVUGIB. The primary outcome was inpatient mortality. Multivariable logistic, linear, and Poisson regression analyses were used to estimate clinical outcomes with a p-value < 0.05 was significant.
Results: There were 3,349,779 hospitalizations with NVUGIB. Mean age was 67 yrs and 53.2% were male. Among the admitted patients, Caucasians were 2,215,345 (66.1%), Blacks were 518,295 (15.5) and other races were 616,137 (18.4%). Subgroup with Caucasians, Blacks and other races had Medicare 70.1% vs 60.3% vs 54.9%, Medicaid 9.4% vs 18.9% vs 15.6%, obesity 14.4% vs 14.9% vs 11%, respectively. All-cause mortality in patients admitted with NVUGIB was 235,385, where subgroup with Caucasians, Blacks and other races had 149,860 (6.8%) vs 34,655 (6.7%) vs 50867 (8.6%). The racial subgroup showed significant primary and secondary outcomes that are presented in Table 1 with comorbidities in Table 2.
Discussion: All obtained results revealed statistical significance and we considered Caucasian population as baseline. Mortality, intensive care services and resource utilization proportion was highest among Asian race followed by Hispanic race then by Black race. Cardiac arrest proportion was highest among Black race followed by Asian race then by Hispanic race. LOS was highest among Asian race followed by Black race then by Hispanic race. Understanding these disparities is essential for improving healthcare equity and ensuring that all patients receive appropriate and equitable care regardless of their racial or ethnic background. Addressing these disparities might involve interventions such as improving access to healthcare services, and culturally competent care, and addressing social determinants of health that disproportionately affect certain racial or ethnic groups.
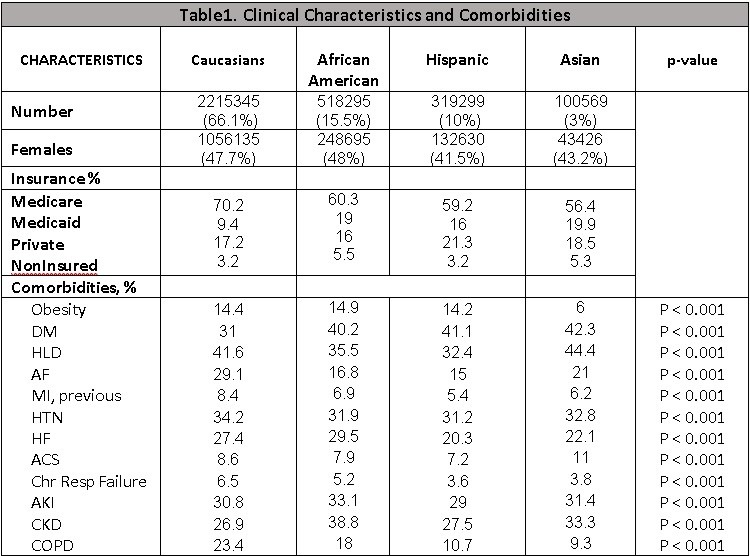
Figure: Image 1
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
M Kenan Rahima indicated no relevant financial relationships.
Mohamad Hijazi indicated no relevant financial relationships.
Mhd Kutaiba Albuni indicated no relevant financial relationships.
Venkata Muddana indicated no relevant financial relationships.
M Kenan Rahima, MD1, Mohamad Hijazi, MD1, Mhd Kutaiba Albuni, MD2, Venkata Muddana, MD3. P4181 - Racial Disparities in Patients With Non-Variceal Upper Gastrointestinal Bleeding in Patients According to a Large National Dataset, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
