Tuesday Poster Session
Category: GI Bleeding
P4199 - Hematemesis in a Patient With Aortic Stent Graft, Coincidence or Not?
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- SS
Simon Sabir, DO
Alameda Health System
Oakland, CA
Presenting Author(s)
Simon Sabir, DO, Jenna Chen, DO, Alejandro Diaz, MD
Alameda Health System, Oakland, CA
Introduction: Aortoenteric fistulas (AEF), aberrant luminal connections between the aorta and a portion of the enteric system, can be a rare sequela of aortic graft placement. Suspicion for and investigation of AEFs are critical, especially if they present with a herald bleed that, without intervention, is a fatal finding.
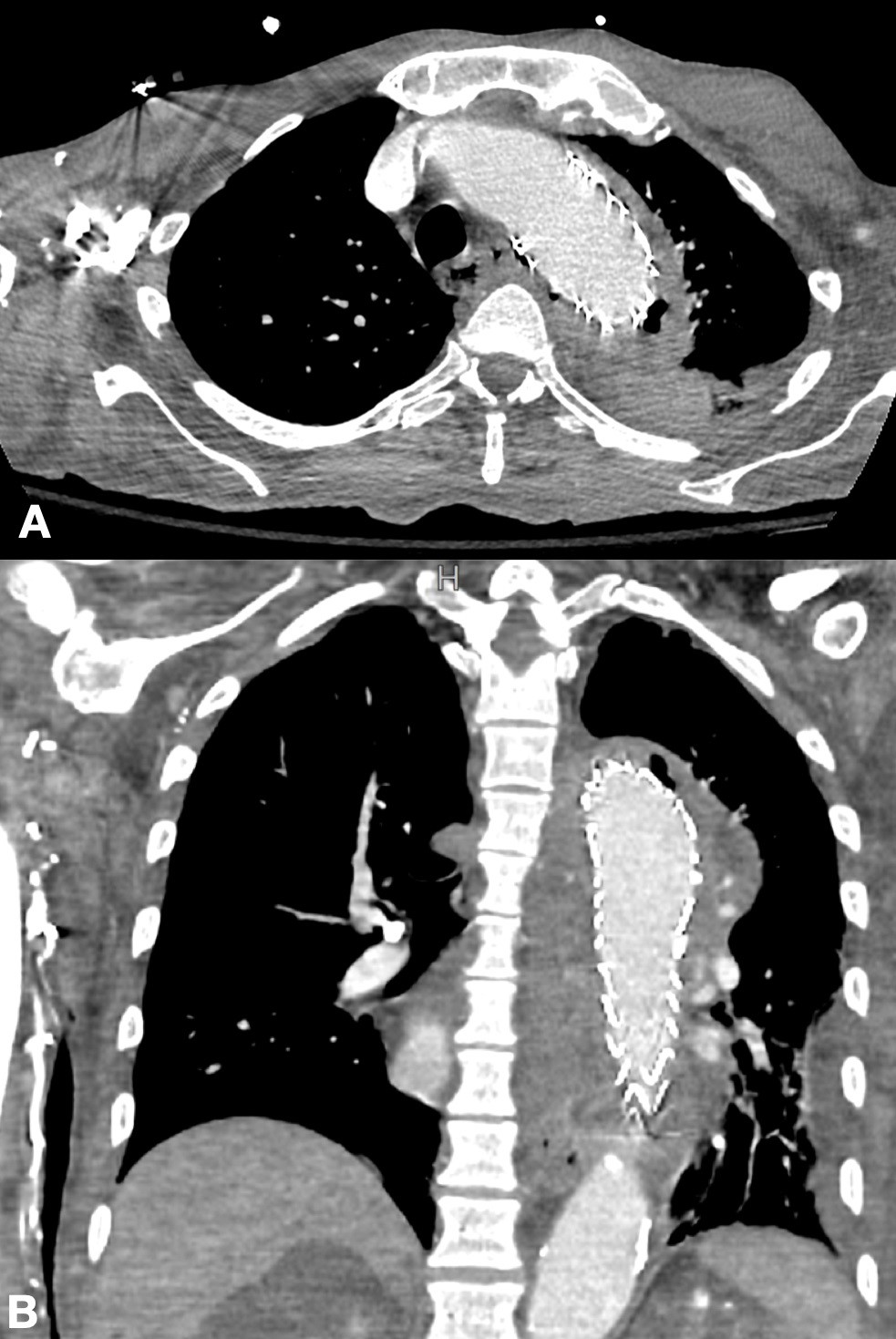
Case Description/Methods: An 80-year-old male with history of descending thoracic aortic ulcer status-post endovascular stent graft and ESRD on hemodialysis presented due to missing dialysis. Notably, the patient presented to the ED days prior for chest pain, and CT dissection protocol confirmed a stable ascending thoracic aorta and patent aortic stent. He again endorsed chest pain at this admission, prompting a repeat CT chest revealing gas adjacent to the stent graft suggesting infection and outpouching of contrast concerning for a leak. Initial management was with IV antibiotics. However, an episode of hematemesis raised concern for developing AEF from the stent graft. EGD was not pursued to avoid manipulation of a possibly compromised esophagus, and he was deemed not a surgical candidate. The patient’s management became solely hemodialysis, antibiotics, and strict blood pressure control. He expired from PEA arrest secondary to hematemesis and aspiration.
Discussion: This case underscores that AEFs should be considered in patients with stent graft and gastrointestinal bleed. AEFs are a rare outcome; one 36-year study showed occurrence in 1.6% of patients who received aortic aneurysm repair. They are often secondary to stent graft, with stent infection, subsequent mass effect, and extravasation into the gut lumen being more common than an aneurysm itself causing AEF. AEFs have reportedly variable timing, occurring two weeks to over 10 years following repair. Mortality is unknown for patients with AEF who do not undergo repair, but it is suspected to be high; 30-day all-cause mortality following AEF repair is reportedly over 40%. Typical presentation is with a herald bleed followed by exsanguination, hence the concern after the patient's initial hematemesis. Management in this case was reasonable, as there is significant 30-day all-cause mortality even with intervention. EGD deferral was also shrewd as it may have thwarted a perforation.
AEFs are rare, but should be considered in patients with hematemesis and a history of aortic stent, regardless of when the stent was placed. If EGD had been pursued in this case, there may have been devastating consequences.
Disclosures:
Simon Sabir, DO, Jenna Chen, DO, Alejandro Diaz, MD. P4199 - Hematemesis in a Patient With Aortic Stent Graft, Coincidence or Not?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Alameda Health System, Oakland, CA
Introduction: Aortoenteric fistulas (AEF), aberrant luminal connections between the aorta and a portion of the enteric system, can be a rare sequela of aortic graft placement. Suspicion for and investigation of AEFs are critical, especially if they present with a herald bleed that, without intervention, is a fatal finding.
Case Description/Methods: An 80-year-old male with history of descending thoracic aortic ulcer status-post endovascular stent graft and ESRD on hemodialysis presented due to missing dialysis. Notably, the patient presented to the ED days prior for chest pain, and CT dissection protocol confirmed a stable ascending thoracic aorta and patent aortic stent. He again endorsed chest pain at this admission, prompting a repeat CT chest revealing gas adjacent to the stent graft suggesting infection and outpouching of contrast concerning for a leak. Initial management was with IV antibiotics. However, an episode of hematemesis raised concern for developing AEF from the stent graft. EGD was not pursued to avoid manipulation of a possibly compromised esophagus, and he was deemed not a surgical candidate. The patient’s management became solely hemodialysis, antibiotics, and strict blood pressure control. He expired from PEA arrest secondary to hematemesis and aspiration.
Discussion: This case underscores that AEFs should be considered in patients with stent graft and gastrointestinal bleed. AEFs are a rare outcome; one 36-year study showed occurrence in 1.6% of patients who received aortic aneurysm repair. They are often secondary to stent graft, with stent infection, subsequent mass effect, and extravasation into the gut lumen being more common than an aneurysm itself causing AEF. AEFs have reportedly variable timing, occurring two weeks to over 10 years following repair. Mortality is unknown for patients with AEF who do not undergo repair, but it is suspected to be high; 30-day all-cause mortality following AEF repair is reportedly over 40%. Typical presentation is with a herald bleed followed by exsanguination, hence the concern after the patient's initial hematemesis. Management in this case was reasonable, as there is significant 30-day all-cause mortality even with intervention. EGD deferral was also shrewd as it may have thwarted a perforation.
AEFs are rare, but should be considered in patients with hematemesis and a history of aortic stent, regardless of when the stent was placed. If EGD had been pursued in this case, there may have been devastating consequences.
Figure: A. Soft tissue thickening and gas surrounding the stented aorta nearly extending into esophagus; transverse
B. Soft tissue thickening and gas surrounding the stented aorta; coronal
B. Soft tissue thickening and gas surrounding the stented aorta; coronal
Disclosures:
Simon Sabir indicated no relevant financial relationships.
Jenna Chen indicated no relevant financial relationships.
Alejandro Diaz indicated no relevant financial relationships.
Simon Sabir, DO, Jenna Chen, DO, Alejandro Diaz, MD. P4199 - Hematemesis in a Patient With Aortic Stent Graft, Coincidence or Not?, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
