Tuesday Poster Session
Category: GI Bleeding
P4202 - Navigating Multi-Site Diverticular Hemorrhage: A Clinical Case Analysis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Alvin B. Newman-Caro, DO
HCA Florida Blake Hospital
Bradenton, FL
Presenting Author(s)
Alvin B. Newman-Caro, DO1, Vikas Sethi, DO2, Janyll Castineira, DO2, Michael Damiano, DO2
1HCA Florida Blake Hospital, Bradenton, FL; 2HCA Florida Largo Hospital, Largo, FL
Introduction: Colonic diverticular hemorrhage is the primary cause of lower gastrointestinal bleeding, affecting 23.9 to 32.5 individuals per 100,000. It originates from the erosion of a blood vessel at the base of a diverticulum. Risk factors for recurrence include NSAID use, obesity, hypertension, and atherosclerosis, with 20% to 35% of patients experiencing a relapse within a year. This presentation highlights the case of a 46-year-old female who underwent multiple endoscopic and endovascular interventions for multi-site diverticular hemorrhage within a 2-month period.
Case Description/Methods: The patient, with a history of colonic diverticulosis and chronic constipation, presented with intermittent bright red blood per rectum for four days. Initial labs showed microcytic hypochromic anemia (hemoglobin 8.1 g/dl), and a CT scan revealed sigmoid diverticulosis without active disease. After bowel preparation, flexible sigmoidoscopy identified active diverticular hemorrhage in the descending colon, treated with epinephrine injection and hemoclips. Despite initial hemostasis, the patient experienced further hematochezia and a drop in hemoglobin the next day. Repeat endoscopy showed continued bleeding. Additional interventions, including hemospray and Purastat, were attempted. Interventional radiology performed emergent embolization, during which another diverticular bleeding site, approximately 10 cm proximal to the first, was identified and treated with an additional coil. Eight weeks later, the patient was readmitted with recurrent hematochezia. Sigmoidoscopy revealed a large blood clot over a bleeding diverticulum, treated again with epinephrine and hemoclips, stabilizing her condition. She was discharged with a recommendation for outpatient surgical evaluation.
Discussion: To effectively pinpoint a diverticular bleed, prioritizing resuscitation, reversing coagulopathies, and evacuating the colon of stool and blood are paramount. Colonoscopy pursued within the initial 15-24 hours enhances the likelihood of identifying stigmata. Endoscopic techniques, such as epinephrine injection and hemoclipping, are common measures used for controlling diverticular bleeding. When identified, current endoscopic techniques can control diverticular bleeding acutely. However, this clinical scenario and the rate of recurrent diverticular hemorrhage emphasize the necessity of exploring more advanced modalities to ensure long-term hemostasis.
Disclosures:
Alvin B. Newman-Caro, DO1, Vikas Sethi, DO2, Janyll Castineira, DO2, Michael Damiano, DO2. P4202 - Navigating Multi-Site Diverticular Hemorrhage: A Clinical Case Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1HCA Florida Blake Hospital, Bradenton, FL; 2HCA Florida Largo Hospital, Largo, FL
Introduction: Colonic diverticular hemorrhage is the primary cause of lower gastrointestinal bleeding, affecting 23.9 to 32.5 individuals per 100,000. It originates from the erosion of a blood vessel at the base of a diverticulum. Risk factors for recurrence include NSAID use, obesity, hypertension, and atherosclerosis, with 20% to 35% of patients experiencing a relapse within a year. This presentation highlights the case of a 46-year-old female who underwent multiple endoscopic and endovascular interventions for multi-site diverticular hemorrhage within a 2-month period.
Case Description/Methods: The patient, with a history of colonic diverticulosis and chronic constipation, presented with intermittent bright red blood per rectum for four days. Initial labs showed microcytic hypochromic anemia (hemoglobin 8.1 g/dl), and a CT scan revealed sigmoid diverticulosis without active disease. After bowel preparation, flexible sigmoidoscopy identified active diverticular hemorrhage in the descending colon, treated with epinephrine injection and hemoclips. Despite initial hemostasis, the patient experienced further hematochezia and a drop in hemoglobin the next day. Repeat endoscopy showed continued bleeding. Additional interventions, including hemospray and Purastat, were attempted. Interventional radiology performed emergent embolization, during which another diverticular bleeding site, approximately 10 cm proximal to the first, was identified and treated with an additional coil. Eight weeks later, the patient was readmitted with recurrent hematochezia. Sigmoidoscopy revealed a large blood clot over a bleeding diverticulum, treated again with epinephrine and hemoclips, stabilizing her condition. She was discharged with a recommendation for outpatient surgical evaluation.
Discussion: To effectively pinpoint a diverticular bleed, prioritizing resuscitation, reversing coagulopathies, and evacuating the colon of stool and blood are paramount. Colonoscopy pursued within the initial 15-24 hours enhances the likelihood of identifying stigmata. Endoscopic techniques, such as epinephrine injection and hemoclipping, are common measures used for controlling diverticular bleeding. When identified, current endoscopic techniques can control diverticular bleeding acutely. However, this clinical scenario and the rate of recurrent diverticular hemorrhage emphasize the necessity of exploring more advanced modalities to ensure long-term hemostasis.
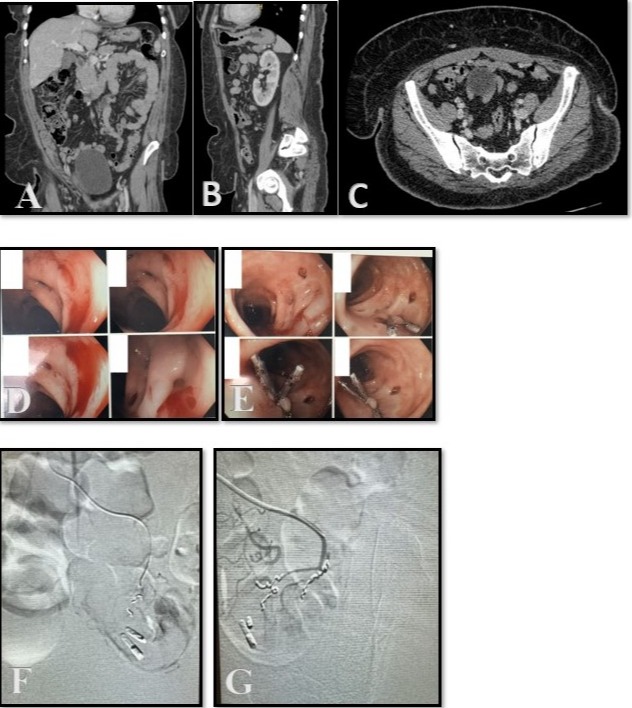
Figure: A,B,C: CT Abdomen/Pelvis with IV Contrast, Coronal/Sagittal/Axial View, demonstrating sigmoid diverticulosis.
D,E: Actively hemorrhaging diverticular bleed with subsequent hemostasis
F,G: Lateral Sigmoid Artery Angiogram
D,E: Actively hemorrhaging diverticular bleed with subsequent hemostasis
F,G: Lateral Sigmoid Artery Angiogram
Disclosures:
Alvin Newman-Caro indicated no relevant financial relationships.
Vikas Sethi indicated no relevant financial relationships.
Janyll Castineira indicated no relevant financial relationships.
Michael Damiano indicated no relevant financial relationships.
Alvin B. Newman-Caro, DO1, Vikas Sethi, DO2, Janyll Castineira, DO2, Michael Damiano, DO2. P4202 - Navigating Multi-Site Diverticular Hemorrhage: A Clinical Case Analysis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
