Tuesday Poster Session
Category: GI Bleeding
P4208 - Uninvited Invader: Gastric Mucormycosis in a Non-Immunocompromised Patient
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mishal Ejaz, MBBS
MedStar Union Memorial Hospital
TOWSON, MD
Presenting Author(s)
Mishal Ejaz, MBBS1, Ishan Kirti, MBBS2, Haider A. Naqvi, MD3, Nahar Saleh, MD1
1MedStar Union Memorial Hospital, Baltimore, MD; 2MedStar Union Memorial Hospital, Towson, MD; 3MedStar Franklin Square Medical Center, Rossville, MD
Introduction: Mucormycosis is a life-threatening fungal infection typically affecting any organ system and may disseminate in severe cases. While common in the immunocompromised, there has recently been a rise in reports of mucormycosis infections in immunocompetent patients. While gastrointestinal (GI) system involvement is less common, numerous cases have been reported in the last decade. This case presents an incidental diagnosis of gastric mucormycosis on EGD for evaluation of anemia, in a patient who was originally admitted for aortic dissection repair.
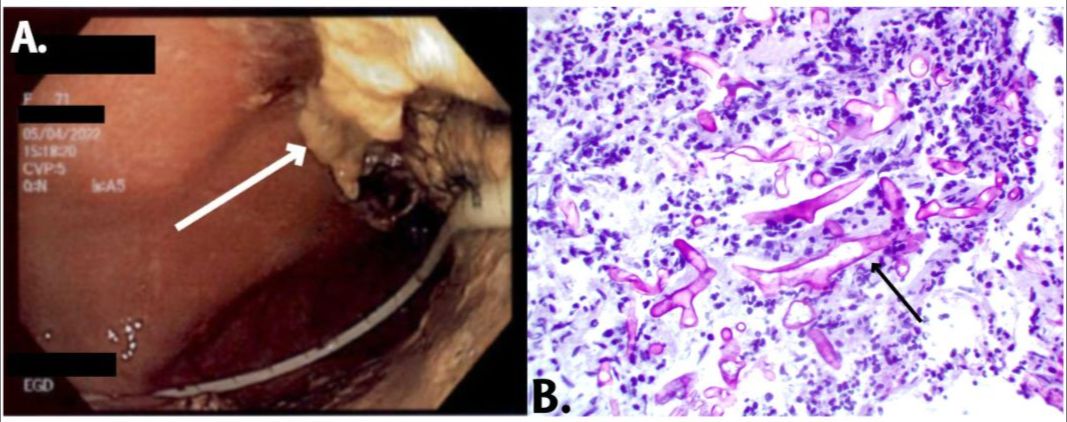
Case Description/Methods: A 71-year-old female was admitted to the hospital for repair of type A aortic dissection. Hospital course was complicated by upper GI bleeding post-repair. During the EGD, the stomach was observed to have adherent yellow material throughout; attempts to remove the mucosa revealed that it scraped easily with a bluish hue. Biopsy revealed fungal hyphal organisms invading the gastric mucosa. The infectious disease (ID) team was consulted, and out of concern for invasive mucormycosis, the patient was started on IV amphotericin B. Initial tissue PCR came back positive for Rhizopus microsporus. After 14 days of therapy, a repeat EGD showed residual patchy abnormal mucosa extending from the fundus to the distal gastric body with areas of ulceration, which was less friable than the initial EGD. Pathology revealed acute on chronic inflammation with granulomatous features without residual fungal organisms. Treatment plan included 8 weeks of IV amphotericin B followed by 6 weeks of PO posaconazole given high mortality rates (~85%). Due to rapid weight loss and failure to thrive, the patient eventually underwent a PEG tube placement.
Discussion: Mucormycosis commonly affects sinuses (39%), lungs (24%), and skin (19%), with the GI tract involved in 7%, primarily the stomach. Symptoms include nonspecific abdominal discomfort, distension, nausea, vomiting, and often bleeding. EGD and biopsy play a critical role in distinguishing mucormycosis from other causes of melena. Antifungal therapy alone is often inadequate for mucormycosis due to poor drug penetration. Surgery to remove infected tissue is typically required for a cure, with studies showing it an independent predictor of favorable outcomes, however, our patient was medically treated successfully. We hope that this case encourages physicians to consider mucormycosis as a potential diagnosis and pursue histologic examination when clinically necessary, even in immunocompetent individuals.
Disclosures:
Mishal Ejaz, MBBS1, Ishan Kirti, MBBS2, Haider A. Naqvi, MD3, Nahar Saleh, MD1. P4208 - Uninvited Invader: Gastric Mucormycosis in a Non-Immunocompromised Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1MedStar Union Memorial Hospital, Baltimore, MD; 2MedStar Union Memorial Hospital, Towson, MD; 3MedStar Franklin Square Medical Center, Rossville, MD
Introduction: Mucormycosis is a life-threatening fungal infection typically affecting any organ system and may disseminate in severe cases. While common in the immunocompromised, there has recently been a rise in reports of mucormycosis infections in immunocompetent patients. While gastrointestinal (GI) system involvement is less common, numerous cases have been reported in the last decade. This case presents an incidental diagnosis of gastric mucormycosis on EGD for evaluation of anemia, in a patient who was originally admitted for aortic dissection repair.
Case Description/Methods: A 71-year-old female was admitted to the hospital for repair of type A aortic dissection. Hospital course was complicated by upper GI bleeding post-repair. During the EGD, the stomach was observed to have adherent yellow material throughout; attempts to remove the mucosa revealed that it scraped easily with a bluish hue. Biopsy revealed fungal hyphal organisms invading the gastric mucosa. The infectious disease (ID) team was consulted, and out of concern for invasive mucormycosis, the patient was started on IV amphotericin B. Initial tissue PCR came back positive for Rhizopus microsporus. After 14 days of therapy, a repeat EGD showed residual patchy abnormal mucosa extending from the fundus to the distal gastric body with areas of ulceration, which was less friable than the initial EGD. Pathology revealed acute on chronic inflammation with granulomatous features without residual fungal organisms. Treatment plan included 8 weeks of IV amphotericin B followed by 6 weeks of PO posaconazole given high mortality rates (~85%). Due to rapid weight loss and failure to thrive, the patient eventually underwent a PEG tube placement.
Discussion: Mucormycosis commonly affects sinuses (39%), lungs (24%), and skin (19%), with the GI tract involved in 7%, primarily the stomach. Symptoms include nonspecific abdominal discomfort, distension, nausea, vomiting, and often bleeding. EGD and biopsy play a critical role in distinguishing mucormycosis from other causes of melena. Antifungal therapy alone is often inadequate for mucormycosis due to poor drug penetration. Surgery to remove infected tissue is typically required for a cure, with studies showing it an independent predictor of favorable outcomes, however, our patient was medically treated successfully. We hope that this case encourages physicians to consider mucormycosis as a potential diagnosis and pursue histologic examination when clinically necessary, even in immunocompetent individuals.
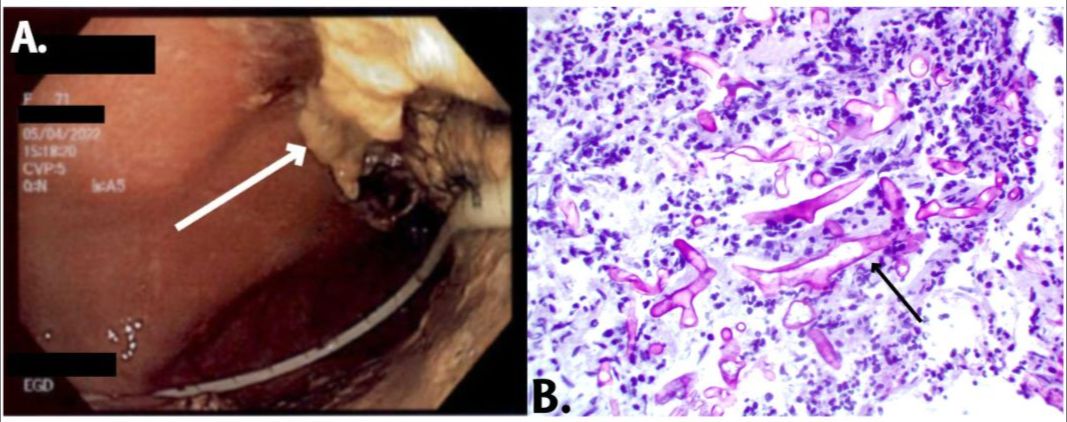
Figure: Fig A. Adherent yellow material throughout gastric mucosa in background of a bluish hue.
Fig B. PAS (fungal) stain, 400x, showing the fungal hyphal organisms (purple/dark pink stained) involving the lamina propria of the stomach and surrounded by inflammatory cells.
Fig B. PAS (fungal) stain, 400x, showing the fungal hyphal organisms (purple/dark pink stained) involving the lamina propria of the stomach and surrounded by inflammatory cells.
Disclosures:
Mishal Ejaz indicated no relevant financial relationships.
Ishan Kirti indicated no relevant financial relationships.
Haider Naqvi indicated no relevant financial relationships.
Nahar Saleh indicated no relevant financial relationships.
Mishal Ejaz, MBBS1, Ishan Kirti, MBBS2, Haider A. Naqvi, MD3, Nahar Saleh, MD1. P4208 - Uninvited Invader: Gastric Mucormycosis in a Non-Immunocompromised Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
