Tuesday Poster Session
Category: GI Bleeding
P4235 - A Rare Case of Gastrointestinal Bleeding Following Atrial Fibrillation Ablation
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- JD
Jake Debroff, MD
Mount Sinai Beth Israel, Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Award: Presidential Poster Award
Jake DeBroff, MD1, Kayla Hartz, DO2, Ayanna Lewis, MD3
1Mount Sinai Beth Israel, Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai Morningside, Icahn School of Medicine at Mount Sinai, Astoria, NY; 3Mount Sinai Morningside and West Hospitals, New York, NY
Introduction: Atrial fibrillation (AF) is a common arrhythmia effecting around 60 million patients annually, and can be treated both medically and with ablation procedures. One rare but dangerous complication of AF ablation is formation of an atrio-esophageal fistula, which occurs in < 0.1 - 0.25% of cases. While an anomalous connection between the left atrium and esophagus may be created by the procedure, other vascular connections can take place iatrogenically. The authors present a case of post-AF ablation gastric and celiac artery bleed.
Case Description/Methods: A 73-year-old male with past history of AF on Eliquis status post direct current cardioversion (DCCV) presented for evaluation of persistent symptomatic AF characterized by presyncope and palpitations. Following a successful pulmonary vein isolation and cavotricuspid isthmus ablation, the patient became hypotensive with two large episodes of hematochezia. His hemoglobin decreased from 15.3 to 10.4g/L, and a total of 2 units of packed red blood cells and a proton pump inhibitor (PPI) were given. Computed Tomography (CT) angiography of the chest and abdomen showed a small blush at the gastroesophageal junction (GEJ).
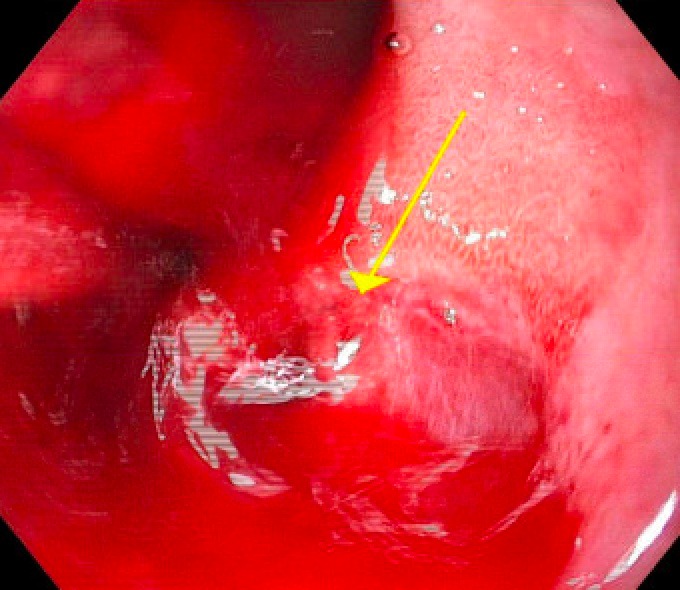
Hematochezia was unresponsive to transfusion support, and hypotension persisted. Urgent esophagogastroduodenoscopy (EGD) revealed ulcerated mucosa at the GEJ with active brisk bleed, and three hemostatic clips were unsuccessfully placed. Interventional radiology subsequently performed celiac angiography showing a large active arterial hemorrhage in the area of the GEJ, followed by successful embolization of the left gastric artery with resolution of bleeding. Patient improved and was discharged on a PPI and close gastroenterology follow up for repeat EGD.
Discussion: Atrio-esophageal fistula is a fatal complication of AF ablation, and the thoracic vasculature adjacent to the esophagus may be vulnerable to trauma. In our case a severe unstable GEJ bleed occurred within 48 hours of the procedure. The gastric and celiac arteries, however, are not typically affected during such procedures. Techniques such as esophageal temperature monitoring and prophylactic PPI use have been suggested for complication prevention. Ultimately, proceduralist experience remains a crucial factor in avoiding such life-threatening complications. GI bleeding events post-ablations should raise clinical suspicion for post-op complications and may warrant urgent endoscopic evaluation. Future studies on prevention of fatal AF ablation complications are warranted.
Disclosures:
Jake DeBroff, MD1, Kayla Hartz, DO2, Ayanna Lewis, MD3. P4235 - A Rare Case of Gastrointestinal Bleeding Following Atrial Fibrillation Ablation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Jake DeBroff, MD1, Kayla Hartz, DO2, Ayanna Lewis, MD3
1Mount Sinai Beth Israel, Icahn School of Medicine at Mount Sinai, New York, NY; 2Mount Sinai Morningside, Icahn School of Medicine at Mount Sinai, Astoria, NY; 3Mount Sinai Morningside and West Hospitals, New York, NY
Introduction: Atrial fibrillation (AF) is a common arrhythmia effecting around 60 million patients annually, and can be treated both medically and with ablation procedures. One rare but dangerous complication of AF ablation is formation of an atrio-esophageal fistula, which occurs in < 0.1 - 0.25% of cases. While an anomalous connection between the left atrium and esophagus may be created by the procedure, other vascular connections can take place iatrogenically. The authors present a case of post-AF ablation gastric and celiac artery bleed.
Case Description/Methods: A 73-year-old male with past history of AF on Eliquis status post direct current cardioversion (DCCV) presented for evaluation of persistent symptomatic AF characterized by presyncope and palpitations. Following a successful pulmonary vein isolation and cavotricuspid isthmus ablation, the patient became hypotensive with two large episodes of hematochezia. His hemoglobin decreased from 15.3 to 10.4g/L, and a total of 2 units of packed red blood cells and a proton pump inhibitor (PPI) were given. Computed Tomography (CT) angiography of the chest and abdomen showed a small blush at the gastroesophageal junction (GEJ).
Hematochezia was unresponsive to transfusion support, and hypotension persisted. Urgent esophagogastroduodenoscopy (EGD) revealed ulcerated mucosa at the GEJ with active brisk bleed, and three hemostatic clips were unsuccessfully placed. Interventional radiology subsequently performed celiac angiography showing a large active arterial hemorrhage in the area of the GEJ, followed by successful embolization of the left gastric artery with resolution of bleeding. Patient improved and was discharged on a PPI and close gastroenterology follow up for repeat EGD.
Discussion: Atrio-esophageal fistula is a fatal complication of AF ablation, and the thoracic vasculature adjacent to the esophagus may be vulnerable to trauma. In our case a severe unstable GEJ bleed occurred within 48 hours of the procedure. The gastric and celiac arteries, however, are not typically affected during such procedures. Techniques such as esophageal temperature monitoring and prophylactic PPI use have been suggested for complication prevention. Ultimately, proceduralist experience remains a crucial factor in avoiding such life-threatening complications. GI bleeding events post-ablations should raise clinical suspicion for post-op complications and may warrant urgent endoscopic evaluation. Future studies on prevention of fatal AF ablation complications are warranted.
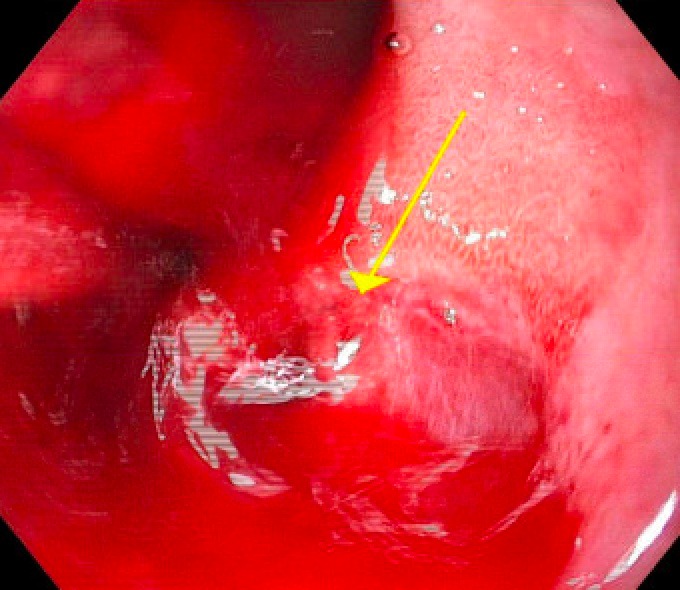
Figure: Endoscopic view of gastroesophageal junction active bleed
Disclosures:
Jake DeBroff indicated no relevant financial relationships.
Kayla Hartz indicated no relevant financial relationships.
Ayanna Lewis indicated no relevant financial relationships.
Jake DeBroff, MD1, Kayla Hartz, DO2, Ayanna Lewis, MD3. P4235 - A Rare Case of Gastrointestinal Bleeding Following Atrial Fibrillation Ablation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

