Tuesday Poster Session
Category: GI Bleeding
P4237 - Twist of Fate: A Gastric Artery Pseudoaneurysm Presenting as Duodenitis
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Rahil Desai, DO
Franciscan Health Olympia Fields
Chicago, IL
Presenting Author(s)
Rahil Desai, DO, Nabiha Haider, DO, Shil Punatar, DO, Shyamal Sheth, DO, Alex Yarbrough, DO
Franciscan Health Olympia Fields, Chicago, IL
Introduction: Gastro-duodenal artery pseudoaneurysms (GDAP) are uncommon but critical sources of upper gastrointestinal bleeding (UGIB) with a significant mortality rate of 21%. GDAPs are often associated with chronic conditions such as pancreatitis (47%), alcohol abuse (25%), and peptic ulcer disease (17%). In this particular case, the GDAP was suspected to be caused by an untreated penetrating duodenal ulcer (DU). Due to the high 75% rupture rate of GDAP, timely intervention is essential; endovascular embolization is the standard treatment. We present a case of GDAP with no associated comorbidities. This case is relevant to add to medical literature as an uncommon case presentation and subsequent management to allow for prompt and early diagnosis.
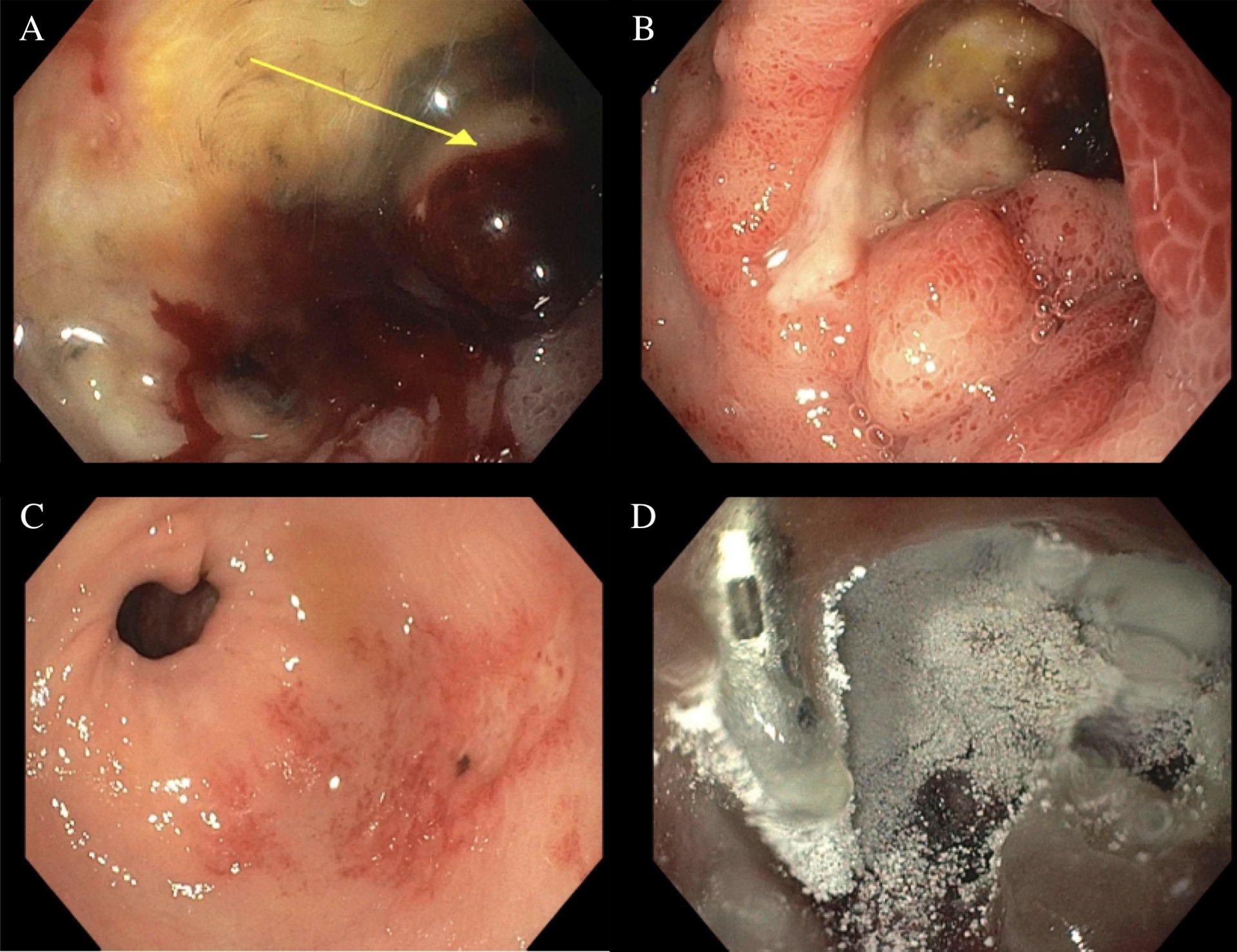
Case Description/Methods: An 83-year-old male with a history of bladder adenocarcinoma s/p cystectomy presented with a 3-day history of melena. Imaging showed changes consistent with duodenitis. He denied NSAID use or iron supplementation. Initial hemoglobin (Hgb) was 9.1, with a baseline of 15. Glascow-Blatchford bleeding score was 15 points, with high concern for an UGIB. Patient was seen by the gastroenterology service with recommendations for urgent esophagogastroduodenoscopy (EGD). EGD showed a pre-pyloric non-bleeding 10mm gastric ulcer with a flat pigmented spot (Forrest Class IIc) and a partially obstructing (60%) non-bleeding, cratered 30mm duodenal ulcer with a non-bleeding visible vessel (Forrest class IIa). Due to the size and location of the ulcers, they were treated with epinephrine and hemostatic spray. A hemostatic clip was placed for localization. After the procedure, the patient’s Hgb declined; this was attributed to friable mucosa and suspected bleeding of a large caliber vessel. Overnight, the patient became hypotensive, requiring fluids, 7u pRBC and 2u platelets. Interventional radiology was emergently contacted; the patient underwent successful coil embolization of a bleeding GDA.
Discussion: GDAP requires high clinical suspicion particularly when presenting as inflammation in surrounding structures. They are an uncommon cause of UGIB and can become life threatening in the presence of large or deep DUs. Recognizing and addressing GDAP promptly can improve outcomes in patients with UGIB and significant DUs. Endovascular embolization is the gold standard of treatment. With this case, we hope to add a step-wise approach, along with interdisciplinary communication with care teams for prompt recognition and management of GDAP.
Disclosures:
Rahil Desai, DO, Nabiha Haider, DO, Shil Punatar, DO, Shyamal Sheth, DO, Alex Yarbrough, DO. P4237 - Twist of Fate: A Gastric Artery Pseudoaneurysm Presenting as Duodenitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Franciscan Health Olympia Fields, Chicago, IL
Introduction: Gastro-duodenal artery pseudoaneurysms (GDAP) are uncommon but critical sources of upper gastrointestinal bleeding (UGIB) with a significant mortality rate of 21%. GDAPs are often associated with chronic conditions such as pancreatitis (47%), alcohol abuse (25%), and peptic ulcer disease (17%). In this particular case, the GDAP was suspected to be caused by an untreated penetrating duodenal ulcer (DU). Due to the high 75% rupture rate of GDAP, timely intervention is essential; endovascular embolization is the standard treatment. We present a case of GDAP with no associated comorbidities. This case is relevant to add to medical literature as an uncommon case presentation and subsequent management to allow for prompt and early diagnosis.
Case Description/Methods: An 83-year-old male with a history of bladder adenocarcinoma s/p cystectomy presented with a 3-day history of melena. Imaging showed changes consistent with duodenitis. He denied NSAID use or iron supplementation. Initial hemoglobin (Hgb) was 9.1, with a baseline of 15. Glascow-Blatchford bleeding score was 15 points, with high concern for an UGIB. Patient was seen by the gastroenterology service with recommendations for urgent esophagogastroduodenoscopy (EGD). EGD showed a pre-pyloric non-bleeding 10mm gastric ulcer with a flat pigmented spot (Forrest Class IIc) and a partially obstructing (60%) non-bleeding, cratered 30mm duodenal ulcer with a non-bleeding visible vessel (Forrest class IIa). Due to the size and location of the ulcers, they were treated with epinephrine and hemostatic spray. A hemostatic clip was placed for localization. After the procedure, the patient’s Hgb declined; this was attributed to friable mucosa and suspected bleeding of a large caliber vessel. Overnight, the patient became hypotensive, requiring fluids, 7u pRBC and 2u platelets. Interventional radiology was emergently contacted; the patient underwent successful coil embolization of a bleeding GDA.
Discussion: GDAP requires high clinical suspicion particularly when presenting as inflammation in surrounding structures. They are an uncommon cause of UGIB and can become life threatening in the presence of large or deep DUs. Recognizing and addressing GDAP promptly can improve outcomes in patients with UGIB and significant DUs. Endovascular embolization is the gold standard of treatment. With this case, we hope to add a step-wise approach, along with interdisciplinary communication with care teams for prompt recognition and management of GDAP.
Figure: A: Partially obstructing (60%) non-bleeding, cratered 30mm duodenal ulcer with a non-bleeding visible vessel (Forrest class IIa)
B: Duodenal bulb with friable mucosa and visible ulcer (Forrest class IIa)
C: Pre-pyloric non-bleeding 10mm gastric ulcer with a flat pigmented spot (Forrest Class IIc)
D: Duodenal ulcer (Forrest class IIa) status-post Epinephrine and hemostatic spray with hemostatic clip placement
B: Duodenal bulb with friable mucosa and visible ulcer (Forrest class IIa)
C: Pre-pyloric non-bleeding 10mm gastric ulcer with a flat pigmented spot (Forrest Class IIc)
D: Duodenal ulcer (Forrest class IIa) status-post Epinephrine and hemostatic spray with hemostatic clip placement
Disclosures:
Rahil Desai indicated no relevant financial relationships.
Nabiha Haider indicated no relevant financial relationships.
Shil Punatar indicated no relevant financial relationships.
Shyamal Sheth indicated no relevant financial relationships.
Alex Yarbrough indicated no relevant financial relationships.
Rahil Desai, DO, Nabiha Haider, DO, Shil Punatar, DO, Shyamal Sheth, DO, Alex Yarbrough, DO. P4237 - Twist of Fate: A Gastric Artery Pseudoaneurysm Presenting as Duodenitis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
