Tuesday Poster Session
Category: GI Bleeding
P4240 - Provocative Testing as a Diagnostic and Therapeutic Tool for Obscure Gastrointestinal Bleeding
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- BA
Binyamin R. Abramowitz, MD
SUNY Downstate Health Sciences University
New York, NY
Presenting Author(s)
Binyamin R. Abramowitz, MD1, Tamta Chkhikvadze, MD2, Bani Chander-Roland, MD, FACG3, Daniel A. DiLeo, MD4
1SUNY Downstate Health Sciences University, New York, NY; 2SUNY Downstate Health Sciences University, Brooklyn, NY; 3VA NY Harbor Health System Clinical Associate Professor SUNY Downstate Health Sciences University, Brooklyn, NY; 4Brooklyn VA Medical Center, Brooklyn, NY
Introduction: Obscure gastrointestinal (GI) bleeding occurs when endoscopic evaluation fails to identify the source of a GI bleed. Patients with obscure GI bleeding experience persistent anemia, recurrent hospitalizations, and numerous endoscopic procedures. Provocative testing employs pharmacological agents to induce bleeding and raise the diagnostic yield of a subsequent endoscopic procedure in a patient with obscure GI bleeding. This technique has not been widely studied and is not commonly utilized. We present a unique case of provocative testing in a patient with obscure GI bleeding with a favorable outcome.
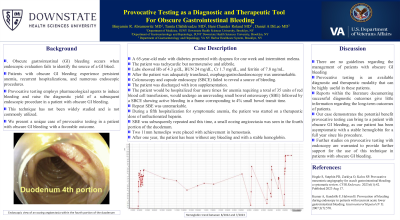
Case Description/Methods: A 65-year-old male with diabetes presented with dyspnea for one week and intermittent melena. The patient was tachycardic but normotensive and afebrile. Labs showed Hb of 4.3 g/dL, BUN 24 mg/dL, Cr 1.7 mg/dL, and ferritin of 7.8 ng/mL. After the patient was adequately transfused, esophagogastroduodenoscopy was unremarkable. Colonoscopy and capsule endoscopy (SBCE) failed to reveal a source of bleeding. The patient was discharged with iron supplementation. The patient would be hospitalized four more times for anemia requiring a total of 35 units of red blood cell transfusions, would undergo an unrevealing small bowel enteroscopy (SBE) followed by a SBCE showing active bleeding in a frame corresponding to 4% small bowel transit time. Repeat SBE was unremarkable. During a fifth hospitalization for symptomatic anemia, the patient was started on a therapeutic dose of unfractionated heparin. SBE was subsequently repeated and this time, a small oozing angioectasia was seen in the fourth portion of the duodenum. Two 11mm hemoclips were placed with achievement in hemostasis. After one year, the patient has been without any bleeding and with a stable hemoglobin.
Discussion: There are no guidelines regarding the management of patients with obscure GI bleeding. Provocative testing is an available diagnostic and therapeutic modality that can be highly useful in these patients. Reports within the literature documenting successful diagnostic outcomes give little information regarding the long-term outcomes of patients. Our case demonstrates the potential benefit provocative testing can bring to a patient with obscure GI bleeding, as our patient has been asymptomatic with a stable hemoglobin for a full year since his procedure. Further studies on provocative testing with endoscopy are warranted to provide further support for the use of this technique in patients with obscure GI bleeding.

Disclosures:
Binyamin R. Abramowitz, MD1, Tamta Chkhikvadze, MD2, Bani Chander-Roland, MD, FACG3, Daniel A. DiLeo, MD4. P4240 - Provocative Testing as a Diagnostic and Therapeutic Tool for Obscure Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1SUNY Downstate Health Sciences University, New York, NY; 2SUNY Downstate Health Sciences University, Brooklyn, NY; 3VA NY Harbor Health System Clinical Associate Professor SUNY Downstate Health Sciences University, Brooklyn, NY; 4Brooklyn VA Medical Center, Brooklyn, NY
Introduction: Obscure gastrointestinal (GI) bleeding occurs when endoscopic evaluation fails to identify the source of a GI bleed. Patients with obscure GI bleeding experience persistent anemia, recurrent hospitalizations, and numerous endoscopic procedures. Provocative testing employs pharmacological agents to induce bleeding and raise the diagnostic yield of a subsequent endoscopic procedure in a patient with obscure GI bleeding. This technique has not been widely studied and is not commonly utilized. We present a unique case of provocative testing in a patient with obscure GI bleeding with a favorable outcome.
Case Description/Methods: A 65-year-old male with diabetes presented with dyspnea for one week and intermittent melena. The patient was tachycardic but normotensive and afebrile. Labs showed Hb of 4.3 g/dL, BUN 24 mg/dL, Cr 1.7 mg/dL, and ferritin of 7.8 ng/mL. After the patient was adequately transfused, esophagogastroduodenoscopy was unremarkable. Colonoscopy and capsule endoscopy (SBCE) failed to reveal a source of bleeding. The patient was discharged with iron supplementation. The patient would be hospitalized four more times for anemia requiring a total of 35 units of red blood cell transfusions, would undergo an unrevealing small bowel enteroscopy (SBE) followed by a SBCE showing active bleeding in a frame corresponding to 4% small bowel transit time. Repeat SBE was unremarkable. During a fifth hospitalization for symptomatic anemia, the patient was started on a therapeutic dose of unfractionated heparin. SBE was subsequently repeated and this time, a small oozing angioectasia was seen in the fourth portion of the duodenum. Two 11mm hemoclips were placed with achievement in hemostasis. After one year, the patient has been without any bleeding and with a stable hemoglobin.
Discussion: There are no guidelines regarding the management of patients with obscure GI bleeding. Provocative testing is an available diagnostic and therapeutic modality that can be highly useful in these patients. Reports within the literature documenting successful diagnostic outcomes give little information regarding the long-term outcomes of patients. Our case demonstrates the potential benefit provocative testing can bring to a patient with obscure GI bleeding, as our patient has been asymptomatic with a stable hemoglobin for a full year since his procedure. Further studies on provocative testing with endoscopy are warranted to provide further support for the use of this technique in patients with obscure GI bleeding.

Figure: Endoscopic view of an oozing angioectasia within the fourth portion of the duodenum
Disclosures:
Binyamin Abramowitz indicated no relevant financial relationships.
Tamta Chkhikvadze indicated no relevant financial relationships.
Bani Chander-Roland indicated no relevant financial relationships.
Daniel DiLeo indicated no relevant financial relationships.
Binyamin R. Abramowitz, MD1, Tamta Chkhikvadze, MD2, Bani Chander-Roland, MD, FACG3, Daniel A. DiLeo, MD4. P4240 - Provocative Testing as a Diagnostic and Therapeutic Tool for Obscure Gastrointestinal Bleeding, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

