Tuesday Poster Session
Category: GI Bleeding
P4221 - Turning Watermelon Into Grapes: GAVE Refractory to Endoscopic Management
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Leah Yao, MD
New York-Presbyterian / Weill Cornell Medical Center
New York, NY
Presenting Author(s)
Leah Yao, MD1, Emily Smith, MD2, Vladislav Fomin, MD1, Sandeep Sikerwar, MD1, David Wan, MD1, Danielle Brandman, MD, MAS1
1New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian/Weill Cornell, New York, NY
Introduction: Gastric antral vascular ectasia (GAVE) is characterized by abnormally dilated blood vessels radiating from the gastric antrum and can cause acute or chronic gastrointestinal (GI) bleeding. GAVE is commonly associated with cirrhosis and portal hypertension, but is distinct from portal hypertensive gastropathy (PHG). This case featured a patient with GAVE, refractory to multiple lines of endoscopic management.
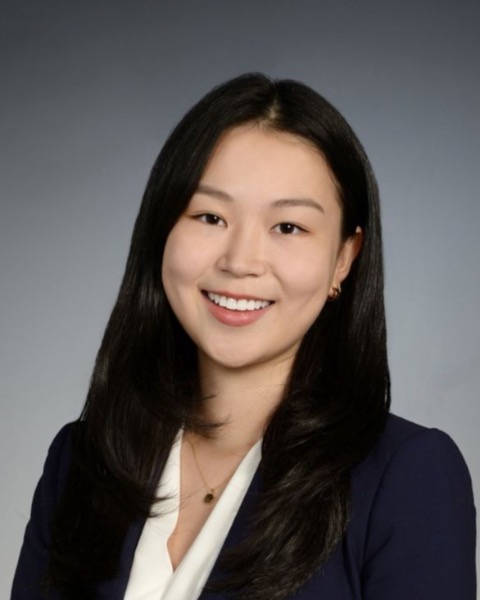
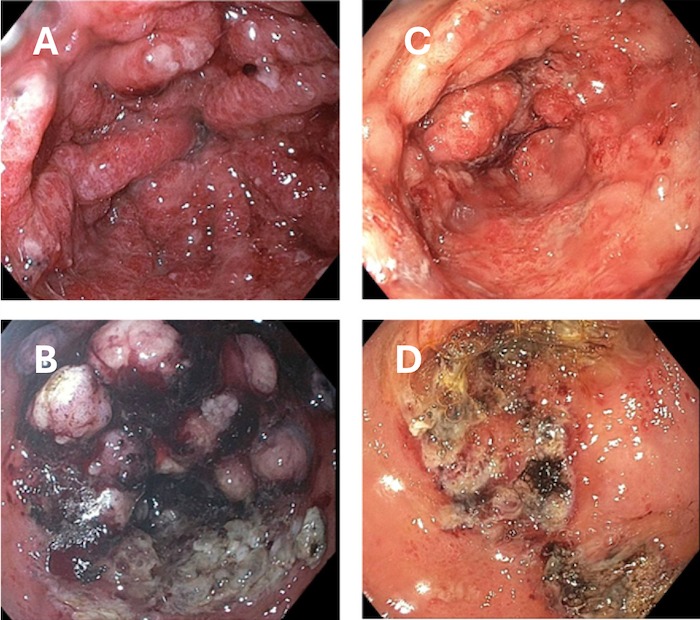
Case Description/Methods: A 69-year-old woman with history of cirrhosis secondary to alcohol use, metabolic associated steatotic liver disease, and GAVE presented with melena, anemia, and hypotension. Over the prior 4 months, she had regular endoscopies (EGDs) performed roughly every 4 weeks for active bleeding and eradication of severe GAVE. She had 17 bands placed on antral nodular GAVE along with repeat argon plasma coagulations (APC). On one EGD, she was found to have a cauliflower-like mass in the gastric antrum, which biopsy confirmed hyperplastic mucosa overlying GAVE. Biopsies of the gastric cardia demonstrated portal hypertensive gastropathy. She required periodic therapeutic paracenteses for worsening ascites during this course. Labs on this admission were notable for Hgb of 4.9 g/dL, AST 42 U/L, ALT 25 U/L, Iron 33 ug/dL. She was transfused and started on octreotide. On repeat EGD, she was found to have significant bleeding from GAVE and was treated with APC. She was medically stabilized with an outpatient plan to start thalidomide and octreotide, continue IV iron infusions, and discuss transjugular intrahepatic portosystemic shunt (TIPS) to treat PHG.
Discussion: Endoscopic management has been the gold standard of treatment of GAVE, with limited prospective literature on medical management. APC is traditionally preferred; however, radiofrequency ablation and endoscopic band ligation (EBL) have also been used for refractory GAVE. Increasing evidence has suggested EBL to have lower recurrent bleeding rates and higher therapeutic success. This patient also developed a hyperplastic polyp overlying GAVE, which along with nodular GAVE differs from the classic linear, flat phenotype and has been associated with the need for repeat APC sessions. While TIPS may help treat this patient’s PHG, surgical antrectomy and liver transplant may be options for refractory GAVE. This case of GAVE highlights the therapeutic challenges in achieving eradication and hemostasis with endoscopic management alone.
Disclosures:
Leah Yao, MD1, Emily Smith, MD2, Vladislav Fomin, MD1, Sandeep Sikerwar, MD1, David Wan, MD1, Danielle Brandman, MD, MAS1. P4221 - Turning Watermelon Into Grapes: GAVE Refractory to Endoscopic Management, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 2New York-Presbyterian/Weill Cornell, New York, NY
Introduction: Gastric antral vascular ectasia (GAVE) is characterized by abnormally dilated blood vessels radiating from the gastric antrum and can cause acute or chronic gastrointestinal (GI) bleeding. GAVE is commonly associated with cirrhosis and portal hypertension, but is distinct from portal hypertensive gastropathy (PHG). This case featured a patient with GAVE, refractory to multiple lines of endoscopic management.
Case Description/Methods: A 69-year-old woman with history of cirrhosis secondary to alcohol use, metabolic associated steatotic liver disease, and GAVE presented with melena, anemia, and hypotension. Over the prior 4 months, she had regular endoscopies (EGDs) performed roughly every 4 weeks for active bleeding and eradication of severe GAVE. She had 17 bands placed on antral nodular GAVE along with repeat argon plasma coagulations (APC). On one EGD, she was found to have a cauliflower-like mass in the gastric antrum, which biopsy confirmed hyperplastic mucosa overlying GAVE. Biopsies of the gastric cardia demonstrated portal hypertensive gastropathy. She required periodic therapeutic paracenteses for worsening ascites during this course. Labs on this admission were notable for Hgb of 4.9 g/dL, AST 42 U/L, ALT 25 U/L, Iron 33 ug/dL. She was transfused and started on octreotide. On repeat EGD, she was found to have significant bleeding from GAVE and was treated with APC. She was medically stabilized with an outpatient plan to start thalidomide and octreotide, continue IV iron infusions, and discuss transjugular intrahepatic portosystemic shunt (TIPS) to treat PHG.
Discussion: Endoscopic management has been the gold standard of treatment of GAVE, with limited prospective literature on medical management. APC is traditionally preferred; however, radiofrequency ablation and endoscopic band ligation (EBL) have also been used for refractory GAVE. Increasing evidence has suggested EBL to have lower recurrent bleeding rates and higher therapeutic success. This patient also developed a hyperplastic polyp overlying GAVE, which along with nodular GAVE differs from the classic linear, flat phenotype and has been associated with the need for repeat APC sessions. While TIPS may help treat this patient’s PHG, surgical antrectomy and liver transplant may be options for refractory GAVE. This case of GAVE highlights the therapeutic challenges in achieving eradication and hemostasis with endoscopic management alone.
Figure: Image 'A' shows GAVE on EGD from 11/22/2023 before EBL & APC.
Image 'B' shows GAVE on EGD from 11/22/2023 after EBL & APC.
Image 'C' shows GAVE on EGD from 2/26/2024 before APC.
Image 'D' shows GAVE on EGD from 2/26/2024 after APC.
Image 'B' shows GAVE on EGD from 11/22/2023 after EBL & APC.
Image 'C' shows GAVE on EGD from 2/26/2024 before APC.
Image 'D' shows GAVE on EGD from 2/26/2024 after APC.
Disclosures:
Leah Yao indicated no relevant financial relationships.
Emily Smith indicated no relevant financial relationships.
Vladislav Fomin indicated no relevant financial relationships.
Sandeep Sikerwar indicated no relevant financial relationships.
David Wan indicated no relevant financial relationships.
Danielle Brandman: Genentech – Grant/Research Support. Gilead – Grant/Research Support.
Leah Yao, MD1, Emily Smith, MD2, Vladislav Fomin, MD1, Sandeep Sikerwar, MD1, David Wan, MD1, Danielle Brandman, MD, MAS1. P4221 - Turning Watermelon Into Grapes: GAVE Refractory to Endoscopic Management, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
