Tuesday Poster Session
Category: General Endoscopy
P4133 - Portal Hypertensive-Polypoid Enteropathy in Cirrhosis: A Case Report
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- JW
Jennifer Wiese, MD
Joan C. Edwards School of Medicine, Marshall University
Huntington, WV
Presenting Author(s)
Jennifer Wiese, MD, Nayiri Derian, MD, Lauren Searls, MD, Maen Kamal, MD
Joan C. Edwards School of Medicine, Marshall University, Huntington, WV
Introduction: Portal hypertensive enteropathy (PHE) describes pathologic mucosal changes observed in the small intestine in a subset of patients with portal hypertension. Polypoid enteropathy is a rare manifestation of PHE with a prevalence of 0.3 %. PHE is commonly a benign finding, however cases with gastrointestinal bleeding, and rare life-threatening outcomes have been reported. No standardized treatment and management exists in the literature.
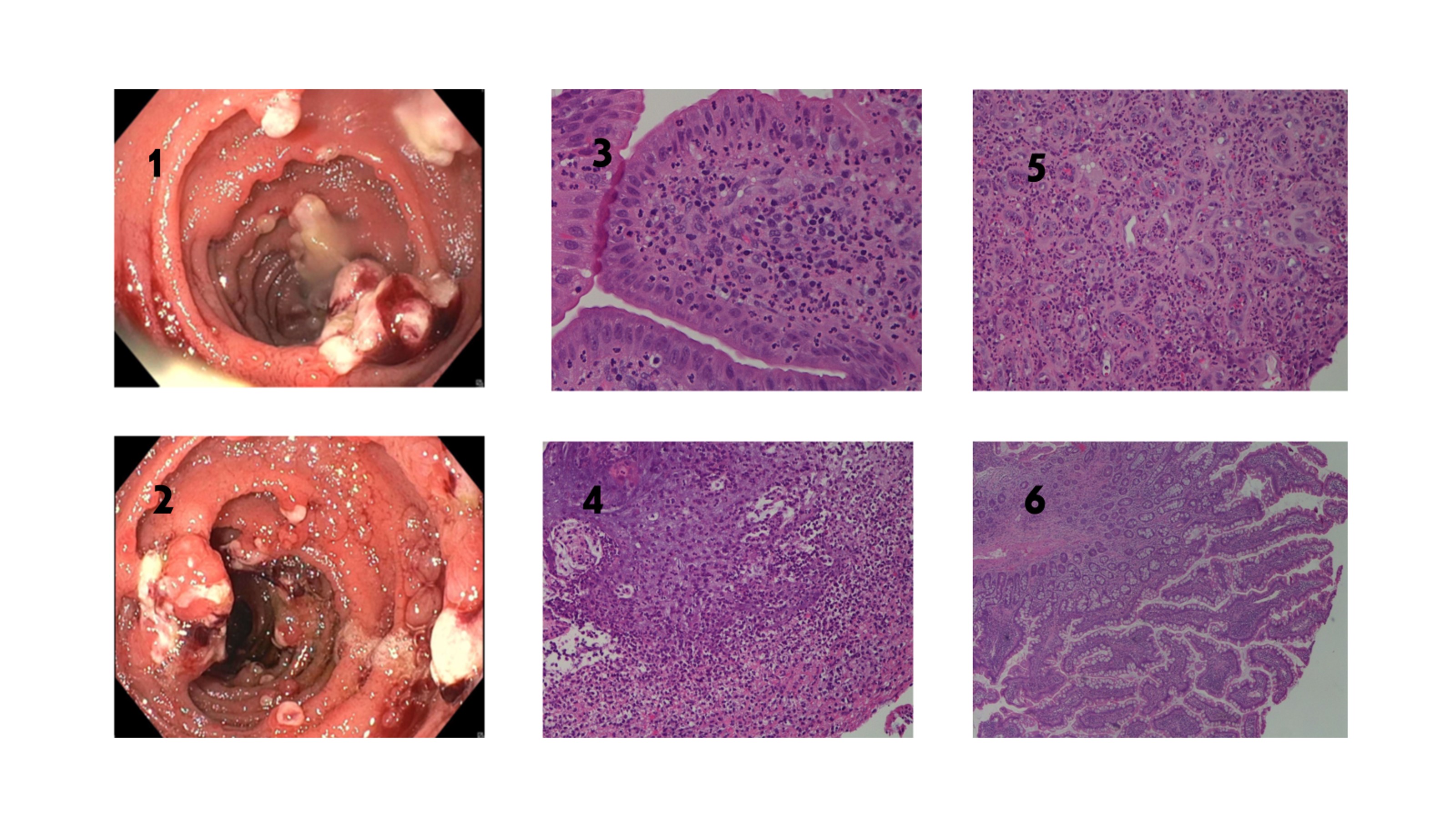
Case Description/Methods: A 43-year-old female with a history of alcohol use disorder, Roux-en-Y gastric bypass presented with abdominal distension, jaundice, and exertional dyspnea. She denied melena, hematochezia, hematemesis, any new or over-the-counter medications. She endorsed alcohol intake of 750 ml vodka daily. Physical exam showed multiple spider nevi, scleral icterus, distended abdomen, hepatomegaly, positive shifting dullness. Laboratory findings revealed macrocytic anemia (Hgb 10.1 gm/dl), mild hyponatremia (133 mEq/L), hypoalbuminemia (1.5 gm/dl), elevated bilirubin (9.1 mg/dl), and INR (1.77). Ultrasound abdomen showed evidence of cirrhotic changes, splenomegaly, and ascites. MELD-NA score was 24 points. Doppler ultrasound findings consistent with portal hypertension (PH). Paracentesis was completed, negative for SBP and malignancy. SAAG value was 1.3 g/dL. Esophagogastroduodenoscopy (EGD) for variceal screening revealed esophageal varices (EV), treated with band ligation, and multiple inflammatory-like jejunal polyps (figure 1, 2), consistent with portal hypertensive jejunal enteropathy. During follow-up EGD, two jejunal polyps were removed using hot snare polypectomy. Histopathology revealed polypoid mucosa with numerous neutrophils in the surface epithelium and lamina propria, active inflammation, vascular proliferation, and granulation tissue, negative for dysplasia or malignancy (figure 3, 4,5, 6).
Discussion: The finding of many inflamed, friable, polypoid lesions during esophageal varices screening in our patient caused a diagnostic and management dilemma. There is limited availability of information on this pathology and treatment options. PHE should be considered in patients with PH who present with gastrointestinal bleeding, especially when portal hypertensive gastropathy and cirrhosis are present. This case highlights a unique patient case and identifies the importance of further studies to evaluate the prevalence, endoscopic classification, and clinical significance of small bowel mucosal changes in patients who have cirrhosis.
Disclosures:
Jennifer Wiese, MD, Nayiri Derian, MD, Lauren Searls, MD, Maen Kamal, MD. P4133 - Portal Hypertensive-Polypoid Enteropathy in Cirrhosis: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Joan C. Edwards School of Medicine, Marshall University, Huntington, WV
Introduction: Portal hypertensive enteropathy (PHE) describes pathologic mucosal changes observed in the small intestine in a subset of patients with portal hypertension. Polypoid enteropathy is a rare manifestation of PHE with a prevalence of 0.3 %. PHE is commonly a benign finding, however cases with gastrointestinal bleeding, and rare life-threatening outcomes have been reported. No standardized treatment and management exists in the literature.
Case Description/Methods: A 43-year-old female with a history of alcohol use disorder, Roux-en-Y gastric bypass presented with abdominal distension, jaundice, and exertional dyspnea. She denied melena, hematochezia, hematemesis, any new or over-the-counter medications. She endorsed alcohol intake of 750 ml vodka daily. Physical exam showed multiple spider nevi, scleral icterus, distended abdomen, hepatomegaly, positive shifting dullness. Laboratory findings revealed macrocytic anemia (Hgb 10.1 gm/dl), mild hyponatremia (133 mEq/L), hypoalbuminemia (1.5 gm/dl), elevated bilirubin (9.1 mg/dl), and INR (1.77). Ultrasound abdomen showed evidence of cirrhotic changes, splenomegaly, and ascites. MELD-NA score was 24 points. Doppler ultrasound findings consistent with portal hypertension (PH). Paracentesis was completed, negative for SBP and malignancy. SAAG value was 1.3 g/dL. Esophagogastroduodenoscopy (EGD) for variceal screening revealed esophageal varices (EV), treated with band ligation, and multiple inflammatory-like jejunal polyps (figure 1, 2), consistent with portal hypertensive jejunal enteropathy. During follow-up EGD, two jejunal polyps were removed using hot snare polypectomy. Histopathology revealed polypoid mucosa with numerous neutrophils in the surface epithelium and lamina propria, active inflammation, vascular proliferation, and granulation tissue, negative for dysplasia or malignancy (figure 3, 4,5, 6).
Discussion: The finding of many inflamed, friable, polypoid lesions during esophageal varices screening in our patient caused a diagnostic and management dilemma. There is limited availability of information on this pathology and treatment options. PHE should be considered in patients with PH who present with gastrointestinal bleeding, especially when portal hypertensive gastropathy and cirrhosis are present. This case highlights a unique patient case and identifies the importance of further studies to evaluate the prevalence, endoscopic classification, and clinical significance of small bowel mucosal changes in patients who have cirrhosis.
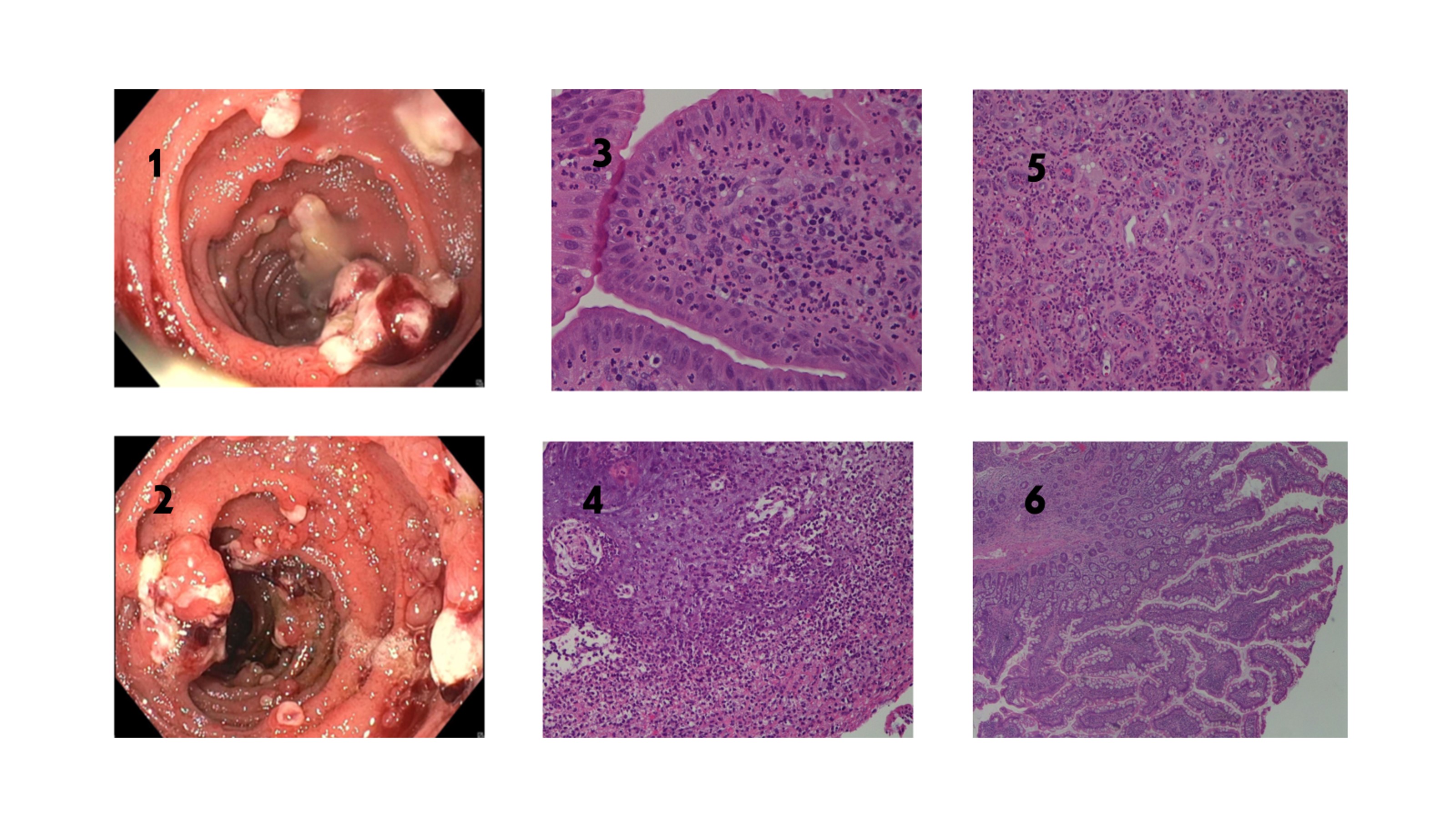
Figure: Figure 1: Multiple inflammatory-like, friable jejunal polyps seen during EGD.
Figure 2: Multiple jejunal polyps seen during EGD
Figure 3: Acute inflammation 20X magnification: Several villi in the small intestinal mucosa show numerous neutrophils in the surface epithelium and lamina propria.
Figure 4: Granulation tissue 20X magnification: The small intestinal stroma shows proliferation of small vessels with numerous acute inflammatory cells
Figure 5: Necrosis 40X magnification: Abundant acute inflammatory cells with evidence of tissue necrosis. Intact and viable small intestinal type mucosa is not identified
Figure 6: Normal mucosa 10X magnification: Low power view of small bowel biopsy shows areas of viable mucosa with intact elongated villi and no significant acute inflammation or necrosis.
Figure 2: Multiple jejunal polyps seen during EGD
Figure 3: Acute inflammation 20X magnification: Several villi in the small intestinal mucosa show numerous neutrophils in the surface epithelium and lamina propria.
Figure 4: Granulation tissue 20X magnification: The small intestinal stroma shows proliferation of small vessels with numerous acute inflammatory cells
Figure 5: Necrosis 40X magnification: Abundant acute inflammatory cells with evidence of tissue necrosis. Intact and viable small intestinal type mucosa is not identified
Figure 6: Normal mucosa 10X magnification: Low power view of small bowel biopsy shows areas of viable mucosa with intact elongated villi and no significant acute inflammation or necrosis.
Disclosures:
Jennifer Wiese indicated no relevant financial relationships.
Nayiri Derian indicated no relevant financial relationships.
Lauren Searls indicated no relevant financial relationships.
Maen Kamal indicated no relevant financial relationships.
Jennifer Wiese, MD, Nayiri Derian, MD, Lauren Searls, MD, Maen Kamal, MD. P4133 - Portal Hypertensive-Polypoid Enteropathy in Cirrhosis: A Case Report, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
