Tuesday Poster Session
Category: General Endoscopy
P4139 - Asymptomatic Intestinal Spirochetosis Associated With Mucosal Abnormalities Discovered on Screening Colonoscopy
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
Brian W. McSteen, MD
New York-Presbyterian / Weill Cornell Medical Center
New York, NY
Presenting Author(s)
Brian W. McSteen, MD1, Lasha Gogokhia, MD1, Annika Windon, MD2, David Wan, MD1
1New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 2Weill Cornell Medicine, New York, NY
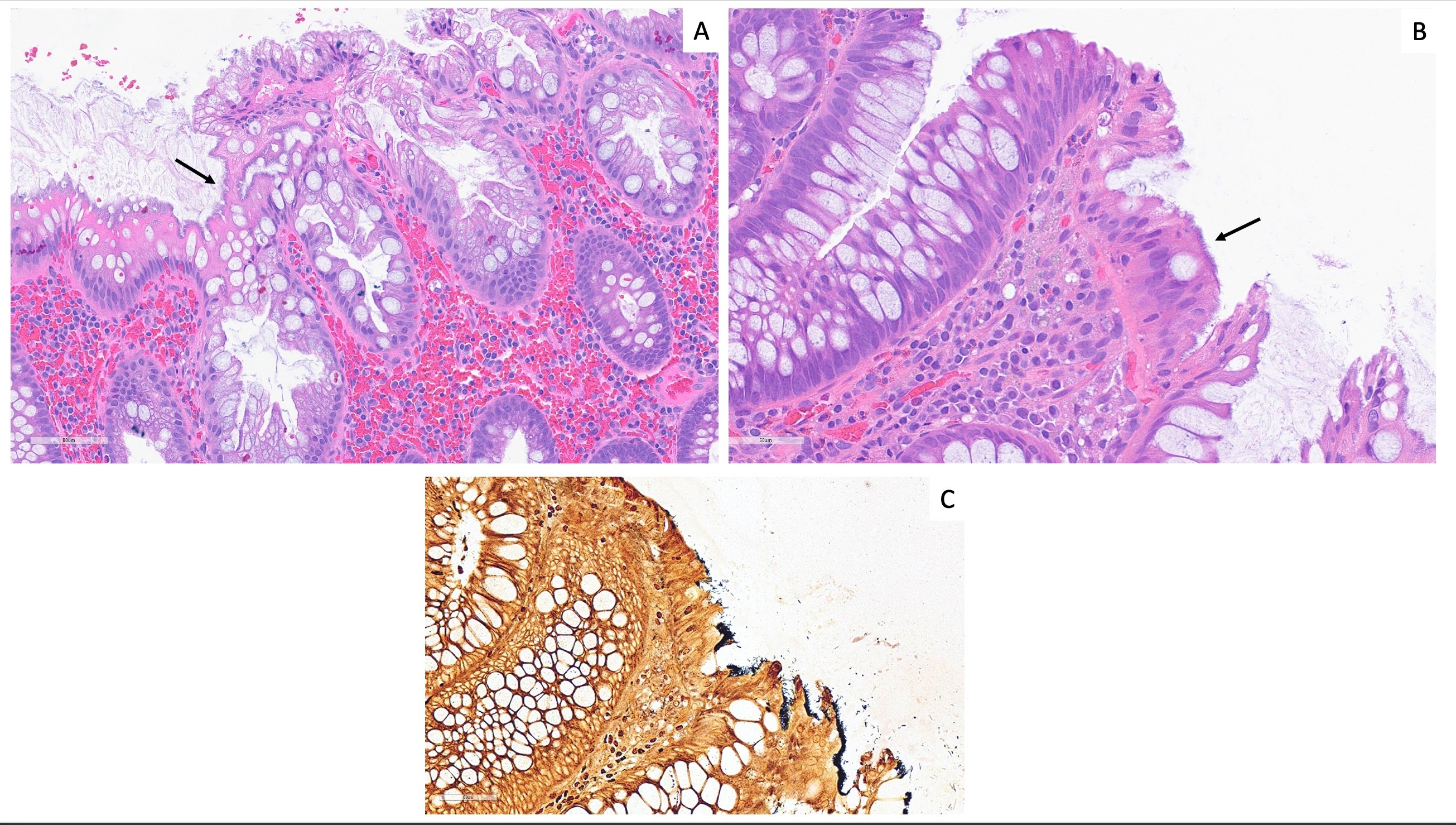
Introduction: Intestinal spirochetosis (IS) is histologically characterized by the presence of spirochetal microorganisms, most commonly Brachyspira aalborgi or Brachyspira pilosicoli, on the apical cell membrane of the rectal or colonic epithelium. Diagnosis is made based on the histologic appearance of a “false brush border” on hematoxylin-eosin staining. The clinical significance of IS is uncertain.
Case Description/Methods: A 55-year-old man with a history of active tobacco use presented for routine screening colonoscopy. Laboratory results 4 months prior to colonoscopy were notable for a white blood cell count of 9.8 (10^3/uL, 3.8-10.8), Hgb 17.5 (g/dL, 13.2-17.1), Mean corpuscle volume 93.2 (fL, 80.0-100.0), rapid plasmin reagin non-reactive (non-reactive). Colonoscopy was notable for four sessile polyps (2 to 5mm in size) in the rectum, recto-sigmoid, sigmoid, and ascending colon, a 15mm sessile polyp in the hepatic flexure, and diverticulosis in the left colon. Pathology showed a sessile serrated polyp (SSP) in the hepatic flexure biopsy, a tubular adenoma (TA) in sigmoid colon and hyperplastic polyps in ascending and rectosigmoid colon. All samples submitted were noted to have associated IS. Warthin-Starry stains were performed on the ascending colon hyperplastic polyp and sigmoid colon tubular adenoma, confirming the diagnosis of IS. The results were shared with the patient who again denied any gastrointestinal symptoms and declined treatment with antibiotics. Given poor colonoscopy preparation, he was planned for repeat colonoscopy in 6 months.
Discussion: IS associated with a TA and SSP, as described in this case, is an unusual finding as spirochete colonization is thought to be discouraged with loss of epithelial microvilli. IS may be associated with irritable bowel syndrome, diarrhea and abdominal pain, but can also be asymptomatic. There are no established treatments for IS; once infection is identified treatment with antibiotics is recommended even if the patient is asymptomatic. Metronidazole therapy has been shown to resolve symptoms and eradicate spirochete colonization. The highest rates of stool colonization have been found in HIV-infected individuals and men who have sex with men; the relationship between immunodeficiency and severity of IS is uncertain. Rates of IS are likely underestimated as diagnosis depends on location of sampling and quality of pathology examination. Further characterization is important to understanding this heterogenous condition.
Disclosures:
Brian W. McSteen, MD1, Lasha Gogokhia, MD1, Annika Windon, MD2, David Wan, MD1. P4139 - Asymptomatic Intestinal Spirochetosis Associated With Mucosal Abnormalities Discovered on Screening Colonoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1New York-Presbyterian / Weill Cornell Medical Center, New York, NY; 2Weill Cornell Medicine, New York, NY
Introduction: Intestinal spirochetosis (IS) is histologically characterized by the presence of spirochetal microorganisms, most commonly Brachyspira aalborgi or Brachyspira pilosicoli, on the apical cell membrane of the rectal or colonic epithelium. Diagnosis is made based on the histologic appearance of a “false brush border” on hematoxylin-eosin staining. The clinical significance of IS is uncertain.
Case Description/Methods: A 55-year-old man with a history of active tobacco use presented for routine screening colonoscopy. Laboratory results 4 months prior to colonoscopy were notable for a white blood cell count of 9.8 (10^3/uL, 3.8-10.8), Hgb 17.5 (g/dL, 13.2-17.1), Mean corpuscle volume 93.2 (fL, 80.0-100.0), rapid plasmin reagin non-reactive (non-reactive). Colonoscopy was notable for four sessile polyps (2 to 5mm in size) in the rectum, recto-sigmoid, sigmoid, and ascending colon, a 15mm sessile polyp in the hepatic flexure, and diverticulosis in the left colon. Pathology showed a sessile serrated polyp (SSP) in the hepatic flexure biopsy, a tubular adenoma (TA) in sigmoid colon and hyperplastic polyps in ascending and rectosigmoid colon. All samples submitted were noted to have associated IS. Warthin-Starry stains were performed on the ascending colon hyperplastic polyp and sigmoid colon tubular adenoma, confirming the diagnosis of IS. The results were shared with the patient who again denied any gastrointestinal symptoms and declined treatment with antibiotics. Given poor colonoscopy preparation, he was planned for repeat colonoscopy in 6 months.
Discussion: IS associated with a TA and SSP, as described in this case, is an unusual finding as spirochete colonization is thought to be discouraged with loss of epithelial microvilli. IS may be associated with irritable bowel syndrome, diarrhea and abdominal pain, but can also be asymptomatic. There are no established treatments for IS; once infection is identified treatment with antibiotics is recommended even if the patient is asymptomatic. Metronidazole therapy has been shown to resolve symptoms and eradicate spirochete colonization. The highest rates of stool colonization have been found in HIV-infected individuals and men who have sex with men; the relationship between immunodeficiency and severity of IS is uncertain. Rates of IS are likely underestimated as diagnosis depends on location of sampling and quality of pathology examination. Further characterization is important to understanding this heterogenous condition.
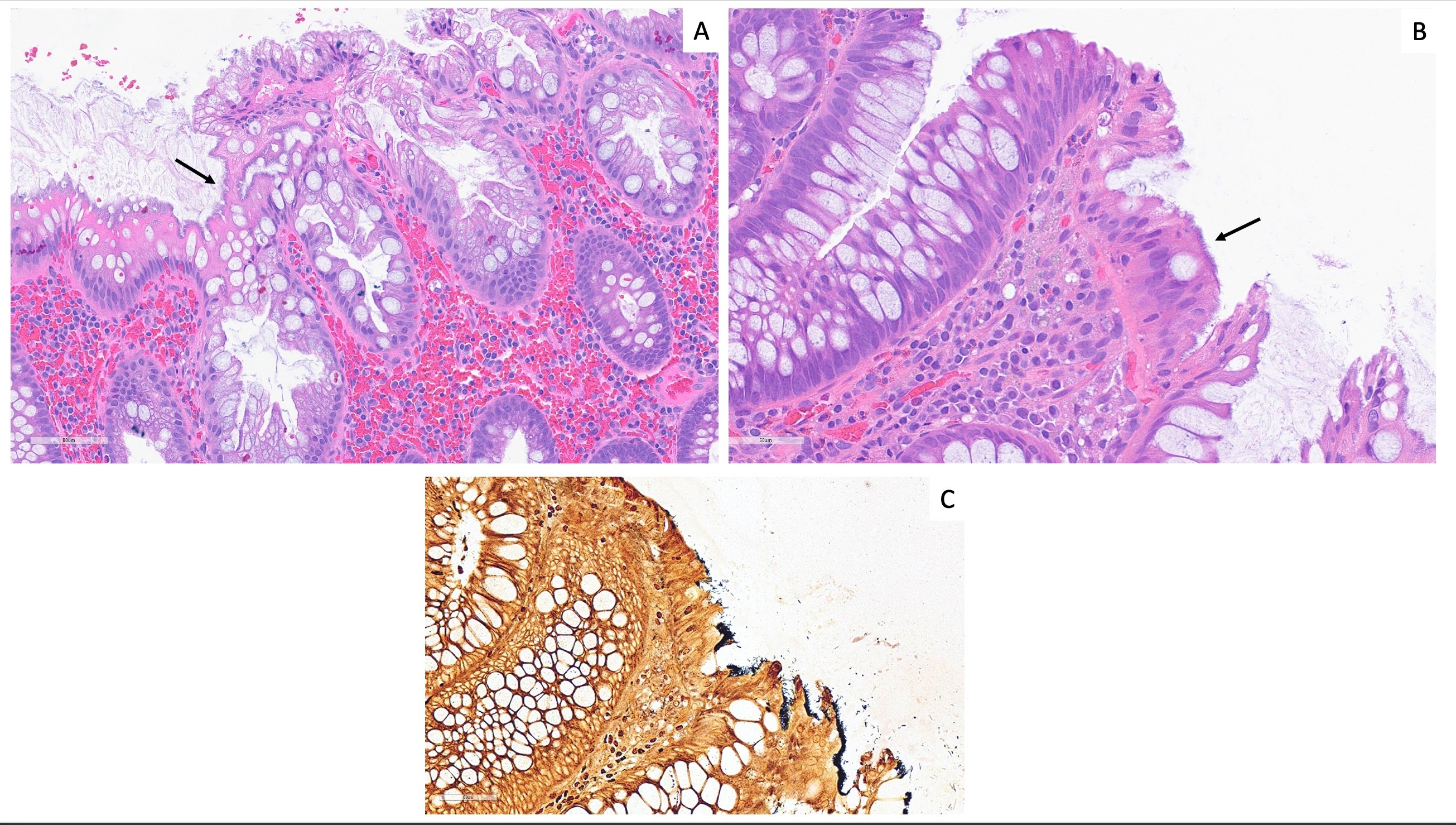
Figure: Intestinal spirochetosis in a sessile serrated polyp (A) and tubular adenoma (B). Hematoxylin and eosin-stained slides highlight a "fuzzy" basophilic border along the luminal surface of the colonic epithelium. The presence of filamentous spirochetes is highlighted by a Warthin-Starry silver stain, creating a black border on the epithelial surface (C).
Disclosures:
Brian McSteen indicated no relevant financial relationships.
Lasha Gogokhia indicated no relevant financial relationships.
Annika Windon indicated no relevant financial relationships.
David Wan indicated no relevant financial relationships.
Brian W. McSteen, MD1, Lasha Gogokhia, MD1, Annika Windon, MD2, David Wan, MD1. P4139 - Asymptomatic Intestinal Spirochetosis Associated With Mucosal Abnormalities Discovered on Screening Colonoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
