Tuesday Poster Session
Category: General Endoscopy
P4142 - Can't Get the GIST of Things: Difficulty Diagnosing and Managing a Bleeding Tumor
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- DW
David Wozny, DO
University of Connecticut
Farmington, CT
Presenting Author(s)
DAVID WOZNY, DO1, Minh Thu T.. Nguyen, MD2, Steven Goldenberg, MD3
1University of Connecticut, Farmington, CT; 2University of Connecticut Health Center, Farmington, CT; 3UConn Health, Hartford, CT
Introduction: Gastrointestinal stromal tumors (GISTs) are mesenchymal neoplasms, constituting 1-2% of primary GI cancers. GISTs originate from the subepithelial layer and often exhibit significant vascularity. Here, we present a rare case of a severely bleeding GIST.
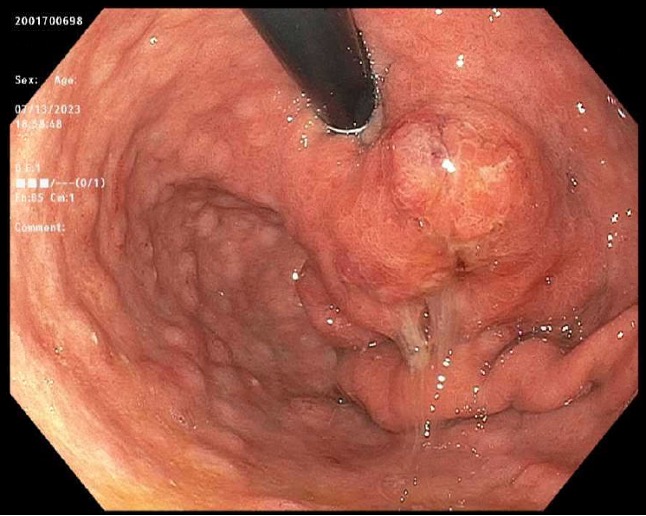
Case Description/Methods: A 72-year-old man presented with acute dizziness, significant hematemesis, and melena. He was stable hemodynamically, with a hemoglobin level of 13.1 g/dL (baseline unknown). CT scan of the chest, abdomen, and pelvis without contrast showed a primary abnormality at the stomach's GE junction, without metastatic disease. Emergent upper endoscopy (EGD) revealed a pulsatile, ulcerated mass in the gastric cardia with active bleeding (Figure 1a). No biopsies were taken due to active bleeding; hemostatic spray was applied. He was transferred to another institution for potential surgery on the mass. Surgery requested tissue diagnosis before proceeding further.
Two days later, his hemoglobin dropped to 11.1 g/dL with new sinus tachycardia. He subsequently underwent EGD with endoscopic ultrasound (EUS), revealing an ulcerated, bleeding gastric cardia treated with hemostatic spray (Figure 1b & 1c). Due to active bleeding, no biopsies were taken once again. The day after bleeding resolved, he had another EGD with forceps biopsy samples yielding "inconclusive" pathology. Five days after the initial EGD, a second EGD/EUS with fine needle aspiration (FNA) confirmed a well-differentiated neuroendocrine tumor, grade 2 GIST (Figure 1d). Hospitalization was further complicated by aspiration, sepsis, and new renal failure necessitating dialysis. Two months later, he underwent partial gastrectomy with clear margins. Postoperative oncology follow-up initially recommended no adjuvant therapy.
Discussion: This case highlights how GIST can present as a significant upper GI bleed, especially in gastric locations known for higher bleeding risks compared to GISTs in the small intestine. Given the large ulcerated, bleeding, and pulsatile mass, along with negative staging scans (suggesting a high pre-test probability for GIST), initial mass resection would have been preferable to multiple, arguably unnecessary procedures to confirm the diagnosis. This approach is justified since surgery was ultimately necessary, and the diagnosis would not alter management in this scenario. Obtaining samples from subepithelial tumors such as GIST can be challenging. EUS with FNA is preferred over superficial forceps biopsy for guided tissue acquisition.
Disclosures:
DAVID WOZNY, DO1, Minh Thu T.. Nguyen, MD2, Steven Goldenberg, MD3. P4142 - Can't Get the GIST of Things: Difficulty Diagnosing and Managing a Bleeding Tumor, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Connecticut, Farmington, CT; 2University of Connecticut Health Center, Farmington, CT; 3UConn Health, Hartford, CT
Introduction: Gastrointestinal stromal tumors (GISTs) are mesenchymal neoplasms, constituting 1-2% of primary GI cancers. GISTs originate from the subepithelial layer and often exhibit significant vascularity. Here, we present a rare case of a severely bleeding GIST.
Case Description/Methods: A 72-year-old man presented with acute dizziness, significant hematemesis, and melena. He was stable hemodynamically, with a hemoglobin level of 13.1 g/dL (baseline unknown). CT scan of the chest, abdomen, and pelvis without contrast showed a primary abnormality at the stomach's GE junction, without metastatic disease. Emergent upper endoscopy (EGD) revealed a pulsatile, ulcerated mass in the gastric cardia with active bleeding (Figure 1a). No biopsies were taken due to active bleeding; hemostatic spray was applied. He was transferred to another institution for potential surgery on the mass. Surgery requested tissue diagnosis before proceeding further.
Two days later, his hemoglobin dropped to 11.1 g/dL with new sinus tachycardia. He subsequently underwent EGD with endoscopic ultrasound (EUS), revealing an ulcerated, bleeding gastric cardia treated with hemostatic spray (Figure 1b & 1c). Due to active bleeding, no biopsies were taken once again. The day after bleeding resolved, he had another EGD with forceps biopsy samples yielding "inconclusive" pathology. Five days after the initial EGD, a second EGD/EUS with fine needle aspiration (FNA) confirmed a well-differentiated neuroendocrine tumor, grade 2 GIST (Figure 1d). Hospitalization was further complicated by aspiration, sepsis, and new renal failure necessitating dialysis. Two months later, he underwent partial gastrectomy with clear margins. Postoperative oncology follow-up initially recommended no adjuvant therapy.
Discussion: This case highlights how GIST can present as a significant upper GI bleed, especially in gastric locations known for higher bleeding risks compared to GISTs in the small intestine. Given the large ulcerated, bleeding, and pulsatile mass, along with negative staging scans (suggesting a high pre-test probability for GIST), initial mass resection would have been preferable to multiple, arguably unnecessary procedures to confirm the diagnosis. This approach is justified since surgery was ultimately necessary, and the diagnosis would not alter management in this scenario. Obtaining samples from subepithelial tumors such as GIST can be challenging. EUS with FNA is preferred over superficial forceps biopsy for guided tissue acquisition.
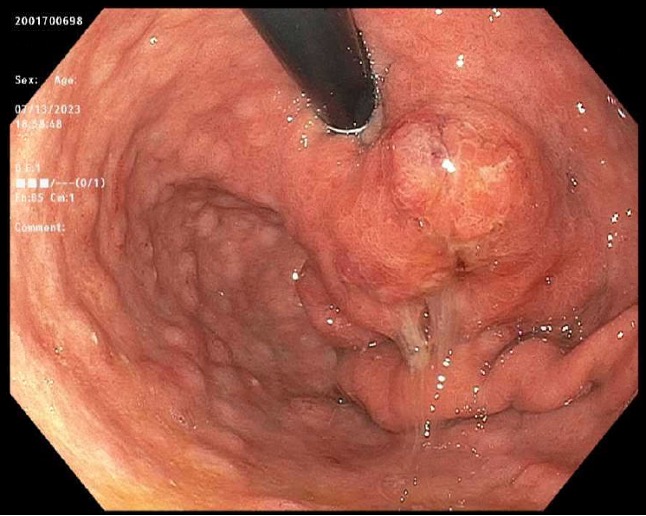
Figure: Figure 1d. Subsequent EGD revealed a gastric antrum mass after the bleeding stigmata had resolved. (Additional Figures include 1a Bleeding Ulcerated Mass, Figure 1b EUS Demonstrating hypervascularity of mass, Figure 1c EUS demonstrating FNA of mass)
Disclosures:
DAVID WOZNY indicated no relevant financial relationships.
Minh Thu Nguyen indicated no relevant financial relationships.
Steven Goldenberg indicated no relevant financial relationships.
DAVID WOZNY, DO1, Minh Thu T.. Nguyen, MD2, Steven Goldenberg, MD3. P4142 - Can't Get the GIST of Things: Difficulty Diagnosing and Managing a Bleeding Tumor, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
