Tuesday Poster Session
Category: General Endoscopy
P4143 - Precipitating Paralysis: An Unexpected Complication After Endoscopy
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- DW
David Wozny, DO
University of Connecticut
Farmington, CT
Presenting Author(s)
DAVID WOZNY, DO1, Minh Thu T.. Nguyen, MD2, Roopjeet K. Bath, MBBS3
1University of Connecticut, Farmington, CT; 2University of Connecticut Health Center, Farmington, CT; 3UConn Health, Farmington, CT
Introduction: We present an unfortunate case of myasthenic crisis following an esophagogastroduodenoscopy (EGD) performed for possible food impaction.
Case Description/Methods: A 41-year-old woman with a history of myasthenia gravis presented to the ED with persistent chest pain. She had discontinued methotrexate and prednisone treatment six months ago after moving. Three weeks prior to presentation, she started having trouble swallowing solid foods, along with fatigue, and heaviness in her legs and arms. On the day of admission, while eating a pork chop, her dysphagia worsened, feeling like food was stuck in her chest.
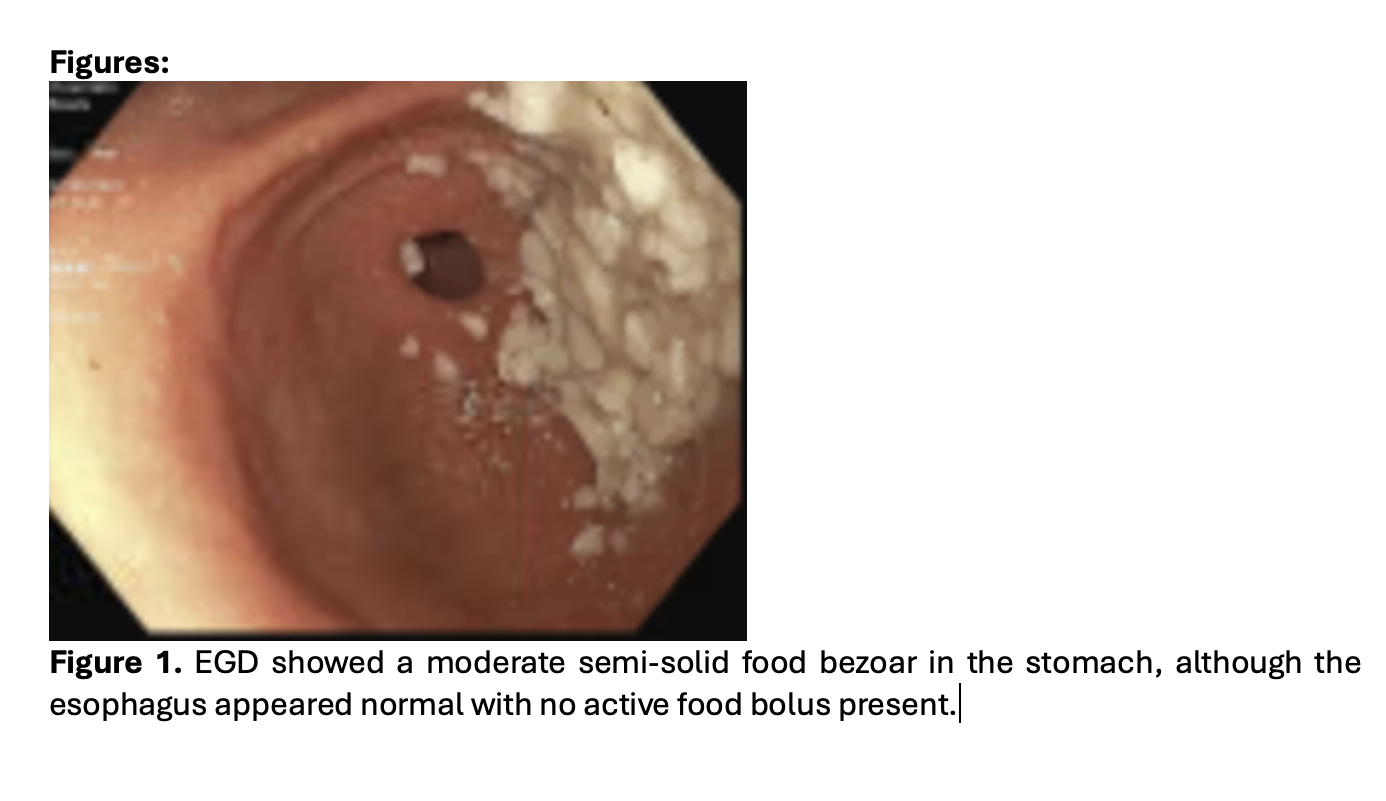
Upon arrival, she was stable without respiratory distress and her basic lab work was normal. Dysphagia due to myasthenia gravis was considered, but due to concern for possible food impaction, she underwent EGD. The anesthesia team intubated which is standard practice for food bolus removal in our hospital. The EGD revealed a moderate amount of food in her stomach, suggesting passage of the obstruction (Fig. 1). The esophagus otherwise appeared normal, but biopsies were performed to exclude eosinophilic esophagitis, with benign pathology results. After initially tolerating the procedure, she developed post-extubation respiratory distress necessitating suctioning due to difficulty managing secretions. Subsequently, she required reintubation for airway protection, indicating a myasthenia crisis that led to ICU admission. Treatment with plasmapheresis, prednisone, and pyridostigmine enabled successful extubation eight days after the EGD.
Discussion: While generally safe, EGD carries various potential complications, including those related to the anesthesia used during the procedure. Our patient experienced a deterioration in myasthenia weakness upon arrival, potentially exacerbated by succinylcholine administration during intubation, intensifying the crisis. While neuromuscular blocking agents and sedatives are crucial for facilitating intubation by inducing muscle relaxation, patients with myasthenia gravis are at increased risk of profound muscle paralysis. Unfortunately, it appears the anesthesia team either did not recognize or inadvertently overlooked the risks associated with succinylcholine in this patient. Implementing changes to the electronic medical record to alert providers about potential medication risks in specific conditions could help prevent similar errors in the future.
Disclosures:
DAVID WOZNY, DO1, Minh Thu T.. Nguyen, MD2, Roopjeet K. Bath, MBBS3. P4143 - Precipitating Paralysis: An Unexpected Complication After Endoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Connecticut, Farmington, CT; 2University of Connecticut Health Center, Farmington, CT; 3UConn Health, Farmington, CT
Introduction: We present an unfortunate case of myasthenic crisis following an esophagogastroduodenoscopy (EGD) performed for possible food impaction.
Case Description/Methods: A 41-year-old woman with a history of myasthenia gravis presented to the ED with persistent chest pain. She had discontinued methotrexate and prednisone treatment six months ago after moving. Three weeks prior to presentation, she started having trouble swallowing solid foods, along with fatigue, and heaviness in her legs and arms. On the day of admission, while eating a pork chop, her dysphagia worsened, feeling like food was stuck in her chest.
Upon arrival, she was stable without respiratory distress and her basic lab work was normal. Dysphagia due to myasthenia gravis was considered, but due to concern for possible food impaction, she underwent EGD. The anesthesia team intubated which is standard practice for food bolus removal in our hospital. The EGD revealed a moderate amount of food in her stomach, suggesting passage of the obstruction (Fig. 1). The esophagus otherwise appeared normal, but biopsies were performed to exclude eosinophilic esophagitis, with benign pathology results. After initially tolerating the procedure, she developed post-extubation respiratory distress necessitating suctioning due to difficulty managing secretions. Subsequently, she required reintubation for airway protection, indicating a myasthenia crisis that led to ICU admission. Treatment with plasmapheresis, prednisone, and pyridostigmine enabled successful extubation eight days after the EGD.
Discussion: While generally safe, EGD carries various potential complications, including those related to the anesthesia used during the procedure. Our patient experienced a deterioration in myasthenia weakness upon arrival, potentially exacerbated by succinylcholine administration during intubation, intensifying the crisis. While neuromuscular blocking agents and sedatives are crucial for facilitating intubation by inducing muscle relaxation, patients with myasthenia gravis are at increased risk of profound muscle paralysis. Unfortunately, it appears the anesthesia team either did not recognize or inadvertently overlooked the risks associated with succinylcholine in this patient. Implementing changes to the electronic medical record to alert providers about potential medication risks in specific conditions could help prevent similar errors in the future.
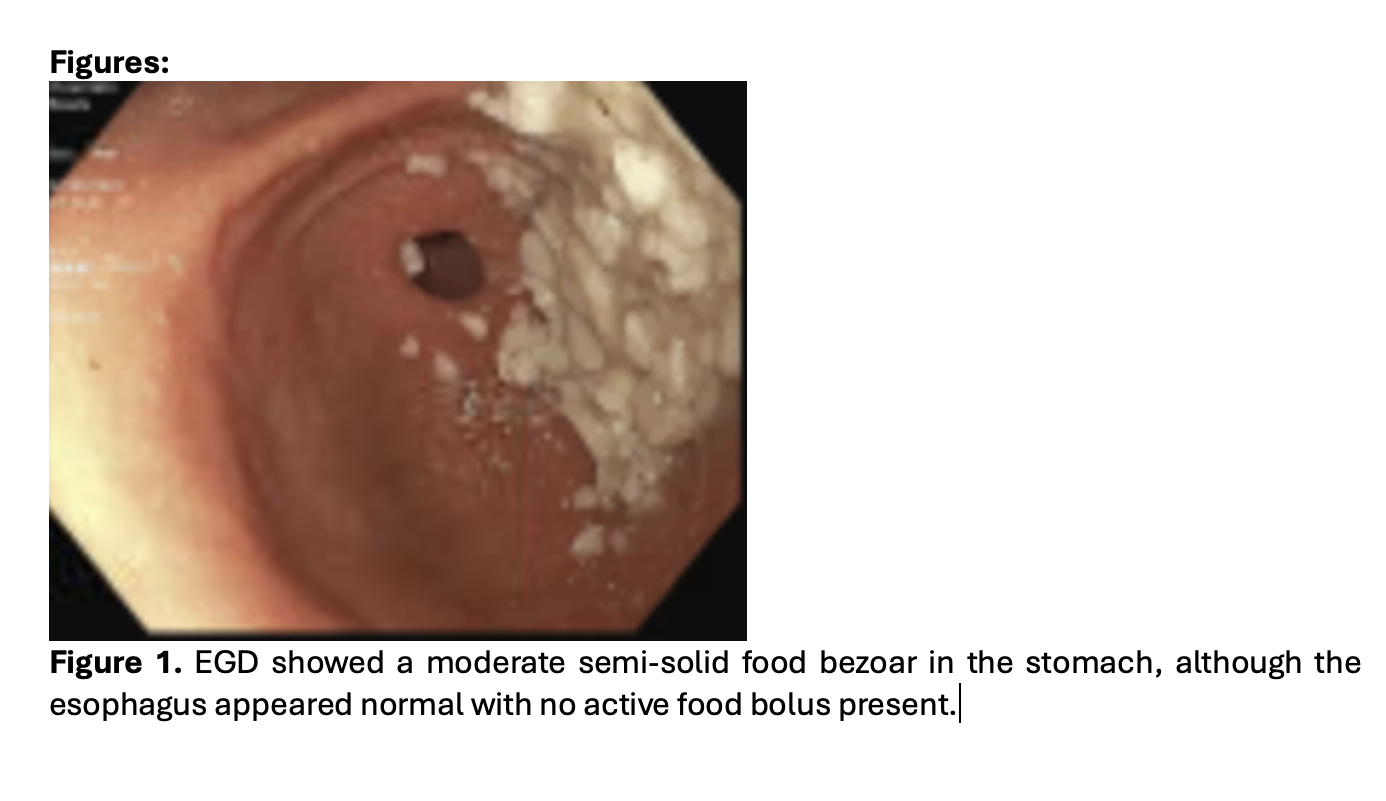
Figure: Figure 1. EGD showed a moderate semi-solid food bezoar in the stomach, although the esophagus appeared normal with no active food bolus present.
Disclosures:
DAVID WOZNY indicated no relevant financial relationships.
Minh Thu Nguyen indicated no relevant financial relationships.
Roopjeet Bath indicated no relevant financial relationships.
DAVID WOZNY, DO1, Minh Thu T.. Nguyen, MD2, Roopjeet K. Bath, MBBS3. P4143 - Precipitating Paralysis: An Unexpected Complication After Endoscopy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
