Tuesday Poster Session
Category: Functional Bowel Disease
P4052 - Utilizing Anorectal Parameters in Pelvic Floor Dyssynergia to Predict Parkinson’s Disease With Implications for Response to Biofeedback
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- KL
Karine Liu, MD
Massachusetts General Hospital
Boston, MA
Presenting Author(s)
Karine Liu, MD1, Karina Oelerich, MD2, Trisha Pasricha, MD, MPH3
1Massachusetts General Hospital, Boston, MA; 2Beth Israel Deaconess Medical Center, Boston, MA; 3BIDMC, Boston, MA
Introduction: Identifying gastrointestinal biomarkers of PD is an area of great interest, and while 80% of PD patients have pelvic floor dyssynergia (PFD), whether particular anorectal manometry (ARM) and PFD symptom parameters can identify PD has not been elucidated. Furthermore, while biofeedback has been effective in treating the general PFD population, its efficacy in PD patients is unclear. We sought to a) study symptom and ARM characteristics and assess their predictive value in distinguishing PD and b) determine the response of biofeedback among PD patients.
Methods: 6 patients with PD-associated PFD were age- and sex- matched to 12 control PFD patients without PD. All met Rome IV criteria for functional constipation, had abnormal balloon expulsion time < 2 minutes and dyssynergia, and completed baseline Patient Assessment of Constipation-Symptoms (PAC-SYM). Of these, 5 PD and 5 matched controls had 8-12 sessions of weekly biofeedback pelvic floor physical therapy. Responders had at least 3 weekly complete spontaneous bowel movements (CSBM) with an increase of 1 weekly CSBM vs. baseline. Continuous and categorical variables were assessed with Student T-tests and Fisher’s exact tests, respectively. We then calculated AUCs and for parameters demonstrating at least moderate clinical utility (AUC > 0.60), assessed optimal cut-off values. The relationship between these criteria and true presence of PD was determined via chi-square tests.
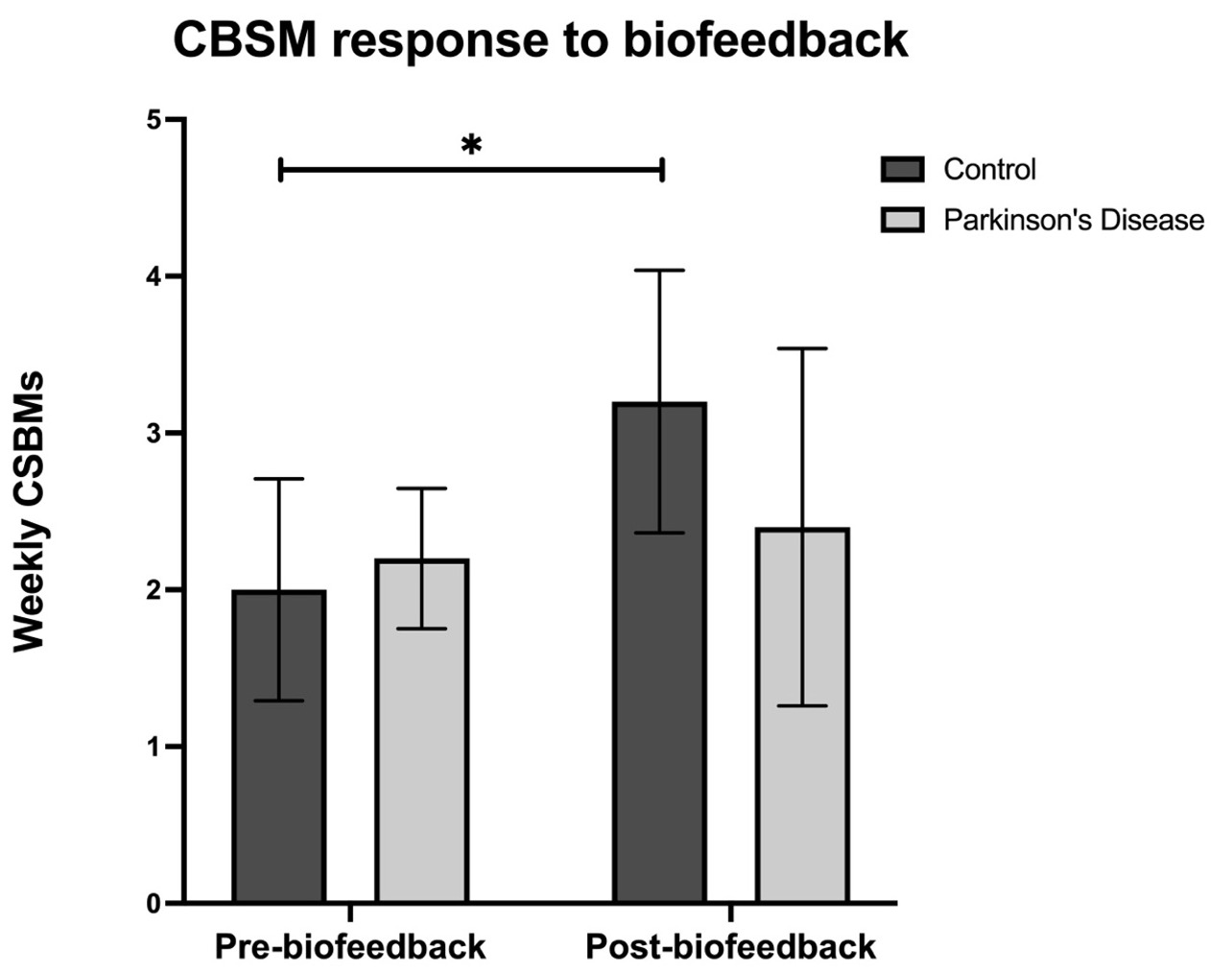
Results: PD patients had significantly lower intra-rectal pressure during bear down and worse stool sub-scores on PAC-SYM. All patients demonstrated first sensation hyposensitivity (Table 1). First sensation pressure, intra-anal pressure during bear down, total PAC-SYM and abdominal sub-scores all individually showed moderate predictive value in identifying PD patients. Notably, after biofeedback, PD patients had minimal improvement in CSBM (2.2 to 2.4, p=.72), 20% responders), while controls improved significantly (2.0 to 3.2, p= .04, 80% responders) (Fig. 2).
Discussion: Our findings preliminarily suggest that symptoms and ARM profiles may be useful to screen for PD in patients with PFD. We also found that PD patients may not respond to biofeedback with the same efficacy as the general population, which may be explained by inadequate rectal pressure increase among PD patients. Further research is needed to validate a predictive model in a larger cohort and determine more precise mechanisms to optimize patient outcomes.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Karine Liu, MD1, Karina Oelerich, MD2, Trisha Pasricha, MD, MPH3. P4052 - Utilizing Anorectal Parameters in Pelvic Floor Dyssynergia to Predict Parkinson’s Disease With Implications for Response to Biofeedback, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Massachusetts General Hospital, Boston, MA; 2Beth Israel Deaconess Medical Center, Boston, MA; 3BIDMC, Boston, MA
Introduction: Identifying gastrointestinal biomarkers of PD is an area of great interest, and while 80% of PD patients have pelvic floor dyssynergia (PFD), whether particular anorectal manometry (ARM) and PFD symptom parameters can identify PD has not been elucidated. Furthermore, while biofeedback has been effective in treating the general PFD population, its efficacy in PD patients is unclear. We sought to a) study symptom and ARM characteristics and assess their predictive value in distinguishing PD and b) determine the response of biofeedback among PD patients.
Methods: 6 patients with PD-associated PFD were age- and sex- matched to 12 control PFD patients without PD. All met Rome IV criteria for functional constipation, had abnormal balloon expulsion time < 2 minutes and dyssynergia, and completed baseline Patient Assessment of Constipation-Symptoms (PAC-SYM). Of these, 5 PD and 5 matched controls had 8-12 sessions of weekly biofeedback pelvic floor physical therapy. Responders had at least 3 weekly complete spontaneous bowel movements (CSBM) with an increase of 1 weekly CSBM vs. baseline. Continuous and categorical variables were assessed with Student T-tests and Fisher’s exact tests, respectively. We then calculated AUCs and for parameters demonstrating at least moderate clinical utility (AUC > 0.60), assessed optimal cut-off values. The relationship between these criteria and true presence of PD was determined via chi-square tests.
Results: PD patients had significantly lower intra-rectal pressure during bear down and worse stool sub-scores on PAC-SYM. All patients demonstrated first sensation hyposensitivity (Table 1). First sensation pressure, intra-anal pressure during bear down, total PAC-SYM and abdominal sub-scores all individually showed moderate predictive value in identifying PD patients. Notably, after biofeedback, PD patients had minimal improvement in CSBM (2.2 to 2.4, p=.72), 20% responders), while controls improved significantly (2.0 to 3.2, p= .04, 80% responders) (Fig. 2).
Discussion: Our findings preliminarily suggest that symptoms and ARM profiles may be useful to screen for PD in patients with PFD. We also found that PD patients may not respond to biofeedback with the same efficacy as the general population, which may be explained by inadequate rectal pressure increase among PD patients. Further research is needed to validate a predictive model in a larger cohort and determine more precise mechanisms to optimize patient outcomes.
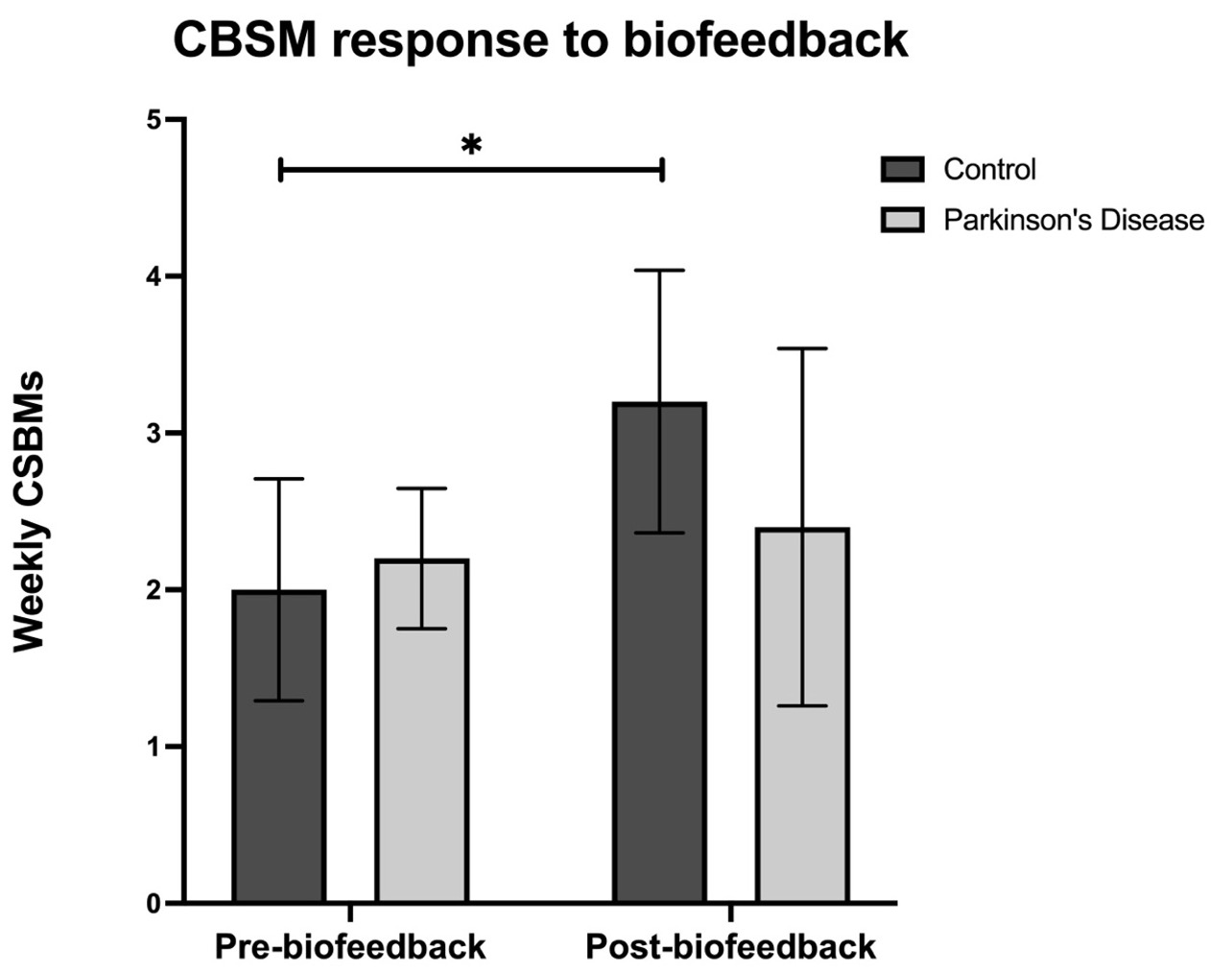
Figure: Figure 1. Differences in response to biofeedback therapy between patients with Parkinson's disease and patients without Parkinson's disease.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Karine Liu indicated no relevant financial relationships.
Karina Oelerich indicated no relevant financial relationships.
Trisha Pasricha indicated no relevant financial relationships.
Karine Liu, MD1, Karina Oelerich, MD2, Trisha Pasricha, MD, MPH3. P4052 - Utilizing Anorectal Parameters in Pelvic Floor Dyssynergia to Predict Parkinson’s Disease With Implications for Response to Biofeedback, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
