Tuesday Poster Session
Category: Functional Bowel Disease
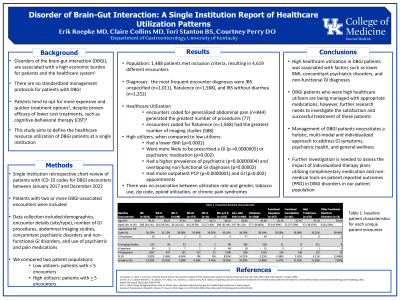
P4060 - Disorder of Brain-Gut interaction: A Single Institution Report of Healthcare Utilization Patterns
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- ER
Erik Roepke, MD
University of Alabama at Birmingham
Birmingham, AL
Presenting Author(s)
Erik Roepke, MD1, Claire Collins, MD2, Tori Stanton, BS2, Courtney Perry, DO, MS2
1University of Alabama at Birmingham, Birmingham, AL; 2University of Kentucky, Lexington, KY
Introduction: Disorders of the brain-gut axis (DBGA), are associated with a high economic burden for patients and the healthcare system. This study aims to define local utilization of healthcare resources by patients with these disorders and better understand variables associated with high healthcare utilization for DGBA diagnoses
Methods: In this retrospective study, we included patients with 2 or more encounters associated with a DBGA ICD-10 code who received care at our institution between 1/2017 to 12/2022. We collected patient demographics, site of healthcare visit, number of gastroenterology (GI) procedures, abdominal imaging, and number and type of GI, psychiatric, and pain medications. We compared high healthcare utilizers ( >5 encounters) to low healthcare utilizers (< 4 encounters).
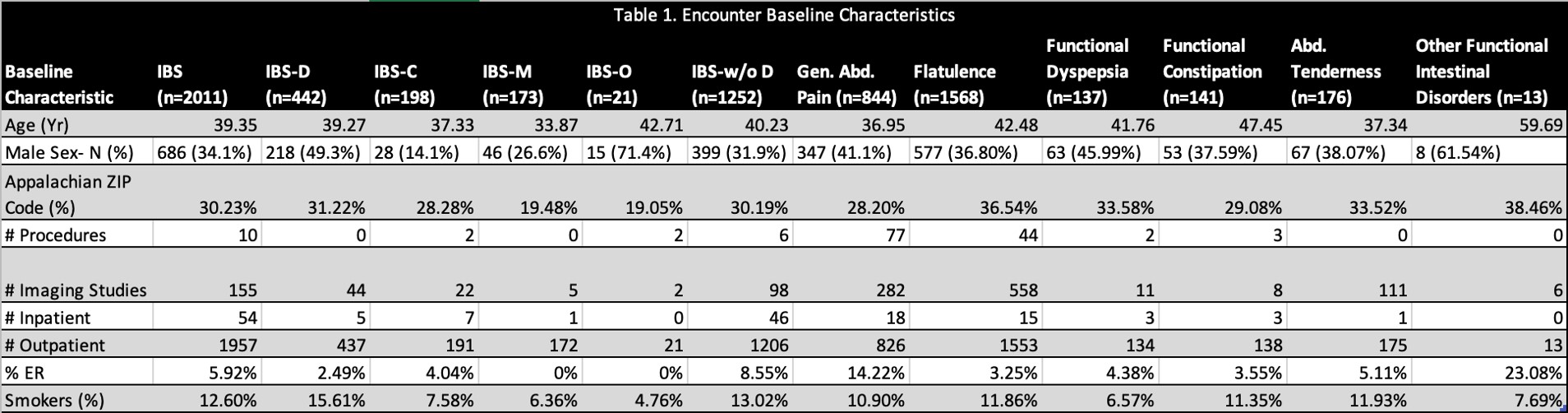
Results: There were 1,488 patients meeting inclusion criteria, accounting for 4619 encounters over the 5-year study period. Most encounters (n=2480) were associated with 1 primary functional diagnosis, while 2139 encounters were coded for 2 or more functional diagnoses. The most commonly coded encounter diagnoses were irritable bowel syndrome unspecified (n=2011), flatulence (n=1568), and irritable bowel syndrome without diarrhea (n=1252). Encounters coded for generalized abdominal pain generated the greatest number of procedures, whereas encounters coded for flatulence had the greatest number of imaging studies. There were 204 patients classified as high healthcare utilizers. There was no association between utilization rate and gender, tobacco use, Appalachian residence, opioid utilization, or chronic pain syndromes. Compared to low utilizers, high utilizers had lower body mass index, were more likely to be prescribed a GI or psychiatric medication, have a psychiatric diagnosis, and an overlapping non-functional GI diagnosis. High utilizers had more general outpatient visits in both outpatient GI and primary care clinic.
Discussion: This study outlined local burden of DGBA and identified factors related to high utilization. We found providers are appropriately utilizing GI and psychiatric medications for this patient population. Further investigations are needed to assess medication adherence, quality of life, satisfaction with clinicians and utilization of complementary medicine and non-medical tools known to positively impact DGBA outcomes.
Disclosures:
Erik Roepke, MD1, Claire Collins, MD2, Tori Stanton, BS2, Courtney Perry, DO, MS2. P4060 - Disorder of Brain-Gut interaction: A Single Institution Report of Healthcare Utilization Patterns, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Alabama at Birmingham, Birmingham, AL; 2University of Kentucky, Lexington, KY
Introduction: Disorders of the brain-gut axis (DBGA), are associated with a high economic burden for patients and the healthcare system. This study aims to define local utilization of healthcare resources by patients with these disorders and better understand variables associated with high healthcare utilization for DGBA diagnoses
Methods: In this retrospective study, we included patients with 2 or more encounters associated with a DBGA ICD-10 code who received care at our institution between 1/2017 to 12/2022. We collected patient demographics, site of healthcare visit, number of gastroenterology (GI) procedures, abdominal imaging, and number and type of GI, psychiatric, and pain medications. We compared high healthcare utilizers ( >5 encounters) to low healthcare utilizers (< 4 encounters).
Results: There were 1,488 patients meeting inclusion criteria, accounting for 4619 encounters over the 5-year study period. Most encounters (n=2480) were associated with 1 primary functional diagnosis, while 2139 encounters were coded for 2 or more functional diagnoses. The most commonly coded encounter diagnoses were irritable bowel syndrome unspecified (n=2011), flatulence (n=1568), and irritable bowel syndrome without diarrhea (n=1252). Encounters coded for generalized abdominal pain generated the greatest number of procedures, whereas encounters coded for flatulence had the greatest number of imaging studies. There were 204 patients classified as high healthcare utilizers. There was no association between utilization rate and gender, tobacco use, Appalachian residence, opioid utilization, or chronic pain syndromes. Compared to low utilizers, high utilizers had lower body mass index, were more likely to be prescribed a GI or psychiatric medication, have a psychiatric diagnosis, and an overlapping non-functional GI diagnosis. High utilizers had more general outpatient visits in both outpatient GI and primary care clinic.
Discussion: This study outlined local burden of DGBA and identified factors related to high utilization. We found providers are appropriately utilizing GI and psychiatric medications for this patient population. Further investigations are needed to assess medication adherence, quality of life, satisfaction with clinicians and utilization of complementary medicine and non-medical tools known to positively impact DGBA outcomes.
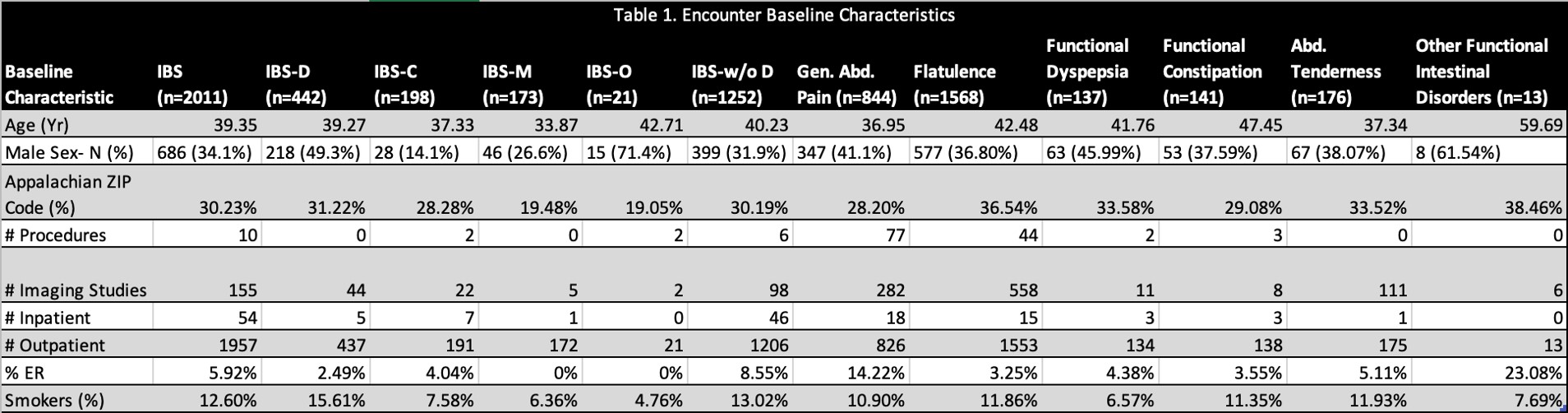
Figure: Table 1. Baseline patient characteristics
Disclosures:
Erik Roepke indicated no relevant financial relationships.
Claire Collins indicated no relevant financial relationships.
Tori Stanton indicated no relevant financial relationships.
Courtney Perry indicated no relevant financial relationships.
Erik Roepke, MD1, Claire Collins, MD2, Tori Stanton, BS2, Courtney Perry, DO, MS2. P4060 - Disorder of Brain-Gut interaction: A Single Institution Report of Healthcare Utilization Patterns, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
