Tuesday Poster Session
Category: Esophagus
P3976 - Unmasking an Obstructive Esophageal Mass: A Rare Case of Esophageal Epithelioid Angiosarcoma Diagnosed With EUS-Guided Biopsy
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Harneet Sangha, BS
Washington State University Elson S. Floyd College of Medicine
Spokane, WA
Presenting Author(s)
Harneet Sangha, BS1, Tavishi Girotra, MBBS2, Shreya Chopra, MBBS2, Navansh Johnson, 2, Anusha Singhania, MBBS2, Mohit Girotra, MD1
1Washington State University Elson S. Floyd College of Medicine, Spokane, WA; 2Digestive Health Institute, Swedish Medical Center, Seattle, WA
Introduction: Gastro-intestinal (GI) angiosarcomas are extremely rare soft tissue tumors arising from endothelial cells of blood and lymphatic vessels and constitute < 1% of all sarcomas. They most commonly originate in the liver and spleen, with occurrences in the small and large intestine being even more uncommon. Epithelioid angiosarcoma (EA) is a morphological variant of angiosarcoma and the etiology remains largely unknown.
We present a case of Esophageal EA in an older man diagnosed via Endoscopic ultrasound (EUS).
Case Description/Methods: A 94-year-old man with hypertension, basal cell carcinoma, previous hip replacement, and subdural hematoma now presented with progressive dysphagia (solids > liquids, 4 months duration and progressive), weight loss of 20 lbs., and shortness of breath. Computed tomography (CT) revealed a large para-esophageal mass/lymph node; however, no clear esophageal narrowing was observed.
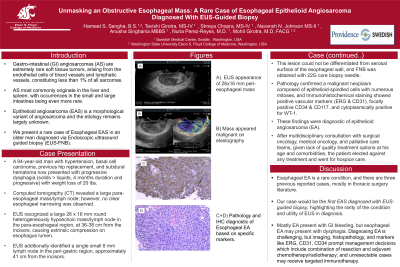
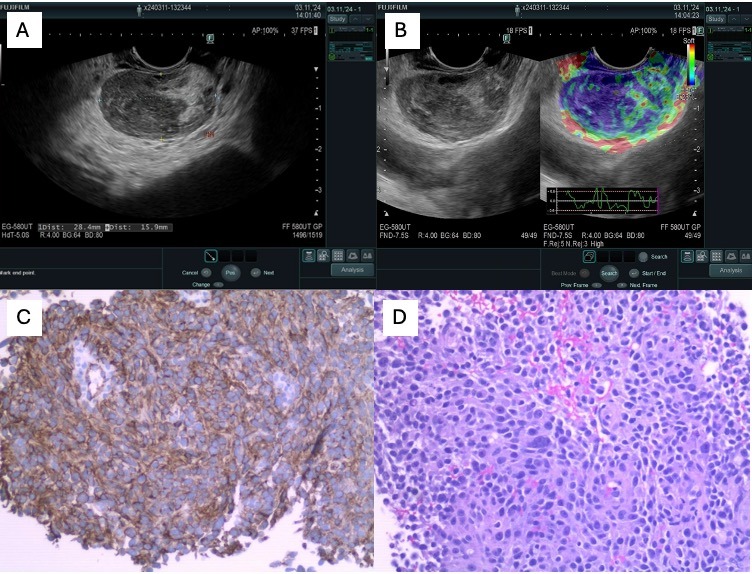
EUS identified a single small 8 mm lymph node in the peri-gastric region, approximately 41 cm from the incisors. Additionally, a large 26x16 mm round heterogeneously hypoechoic mass/lymph node was noted in the para-esophageal region, at 36-38 cm from the incisors, causing extrinsic compression on esophagus lumen. This lesion could not be differentiated from serosal surface of the esophageal wall, and FNB was obtained with 22G core needle.
Pathology confirmed a malignant neoplasm composed of epithelioid-spindled cells with numerous mitoses, and Immunohistochemical staining showed positive vascular markers (ERG & CD31), focally positive CD34 & CD117, and cytoplasmically positive for WT-1. These findings were diagnostic of epithelioid angiosarcoma (EA).
After multidisciplinary consultation with surgical oncology, medical oncology, and palliative care teams, given lack of quality treatment options at his age and comorbidities, the patient elected for hospice.
Discussion: Esophageal EA is a rare condition, and there are three previous reported cases, mostly in thoracic surgery literature.
Our case would be the first diagnosed with EUS-guided biopsy, highlighting the rarity of the condition and utility of EUS in diagnosis.
Mostly EA present with GI bleeding, but esophageal EA may present with dysphagia. Diagnosing EA is challenging, but imaging, histopathology, and markers like ERG, CD31, CD34 prompt management decisions which include combination of resection and adjuvant chemotherapy/radiotherapy; and unresectable cases may receive targeted immunotherapy.
Disclosures:
Harneet Sangha, BS1, Tavishi Girotra, MBBS2, Shreya Chopra, MBBS2, Navansh Johnson, 2, Anusha Singhania, MBBS2, Mohit Girotra, MD1. P3976 - Unmasking an Obstructive Esophageal Mass: A Rare Case of Esophageal Epithelioid Angiosarcoma Diagnosed With EUS-Guided Biopsy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Washington State University Elson S. Floyd College of Medicine, Spokane, WA; 2Digestive Health Institute, Swedish Medical Center, Seattle, WA
Introduction: Gastro-intestinal (GI) angiosarcomas are extremely rare soft tissue tumors arising from endothelial cells of blood and lymphatic vessels and constitute < 1% of all sarcomas. They most commonly originate in the liver and spleen, with occurrences in the small and large intestine being even more uncommon. Epithelioid angiosarcoma (EA) is a morphological variant of angiosarcoma and the etiology remains largely unknown.
We present a case of Esophageal EA in an older man diagnosed via Endoscopic ultrasound (EUS).
Case Description/Methods: A 94-year-old man with hypertension, basal cell carcinoma, previous hip replacement, and subdural hematoma now presented with progressive dysphagia (solids > liquids, 4 months duration and progressive), weight loss of 20 lbs., and shortness of breath. Computed tomography (CT) revealed a large para-esophageal mass/lymph node; however, no clear esophageal narrowing was observed.
EUS identified a single small 8 mm lymph node in the peri-gastric region, approximately 41 cm from the incisors. Additionally, a large 26x16 mm round heterogeneously hypoechoic mass/lymph node was noted in the para-esophageal region, at 36-38 cm from the incisors, causing extrinsic compression on esophagus lumen. This lesion could not be differentiated from serosal surface of the esophageal wall, and FNB was obtained with 22G core needle.
Pathology confirmed a malignant neoplasm composed of epithelioid-spindled cells with numerous mitoses, and Immunohistochemical staining showed positive vascular markers (ERG & CD31), focally positive CD34 & CD117, and cytoplasmically positive for WT-1. These findings were diagnostic of epithelioid angiosarcoma (EA).
After multidisciplinary consultation with surgical oncology, medical oncology, and palliative care teams, given lack of quality treatment options at his age and comorbidities, the patient elected for hospice.
Discussion: Esophageal EA is a rare condition, and there are three previous reported cases, mostly in thoracic surgery literature.
Our case would be the first diagnosed with EUS-guided biopsy, highlighting the rarity of the condition and utility of EUS in diagnosis.
Mostly EA present with GI bleeding, but esophageal EA may present with dysphagia. Diagnosing EA is challenging, but imaging, histopathology, and markers like ERG, CD31, CD34 prompt management decisions which include combination of resection and adjuvant chemotherapy/radiotherapy; and unresectable cases may receive targeted immunotherapy.
Figure: A: EUS appearance of 26x16 mm peri-esophageal mass; B: Mass appeared malignant on elastography; C and D: Pathology and IHC diagnostic of Esophageal EA based on specific markers.
Disclosures:
Harneet Sangha indicated no relevant financial relationships.
Tavishi Girotra indicated no relevant financial relationships.
Shreya Chopra indicated no relevant financial relationships.
Navansh Johnson indicated no relevant financial relationships.
Anusha Singhania indicated no relevant financial relationships.
Mohit Girotra indicated no relevant financial relationships.
Harneet Sangha, BS1, Tavishi Girotra, MBBS2, Shreya Chopra, MBBS2, Navansh Johnson, 2, Anusha Singhania, MBBS2, Mohit Girotra, MD1. P3976 - Unmasking an Obstructive Esophageal Mass: A Rare Case of Esophageal Epithelioid Angiosarcoma Diagnosed With EUS-Guided Biopsy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

