Tuesday Poster Session
Category: Esophagus
P3979 - A Silent Risk: a Case of Esophageal Epidermoid Metaplasia
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E

Has Audio

Suvithan Rajadurai, MD
Brown Medicine/Lifespan
Providence, RI
Presenting Author(s)
Suvithan Rajadurai, MD1, Syed Quadri, MD2, Daniel Greenwald, MD3, Samir Shah, MD3
1Brown University / Rhode Island Hospital, Providence, RI; 2Brown Medicine/Lifespan, Providence, RI; 3Gastroenterology Associates, Providence, RI
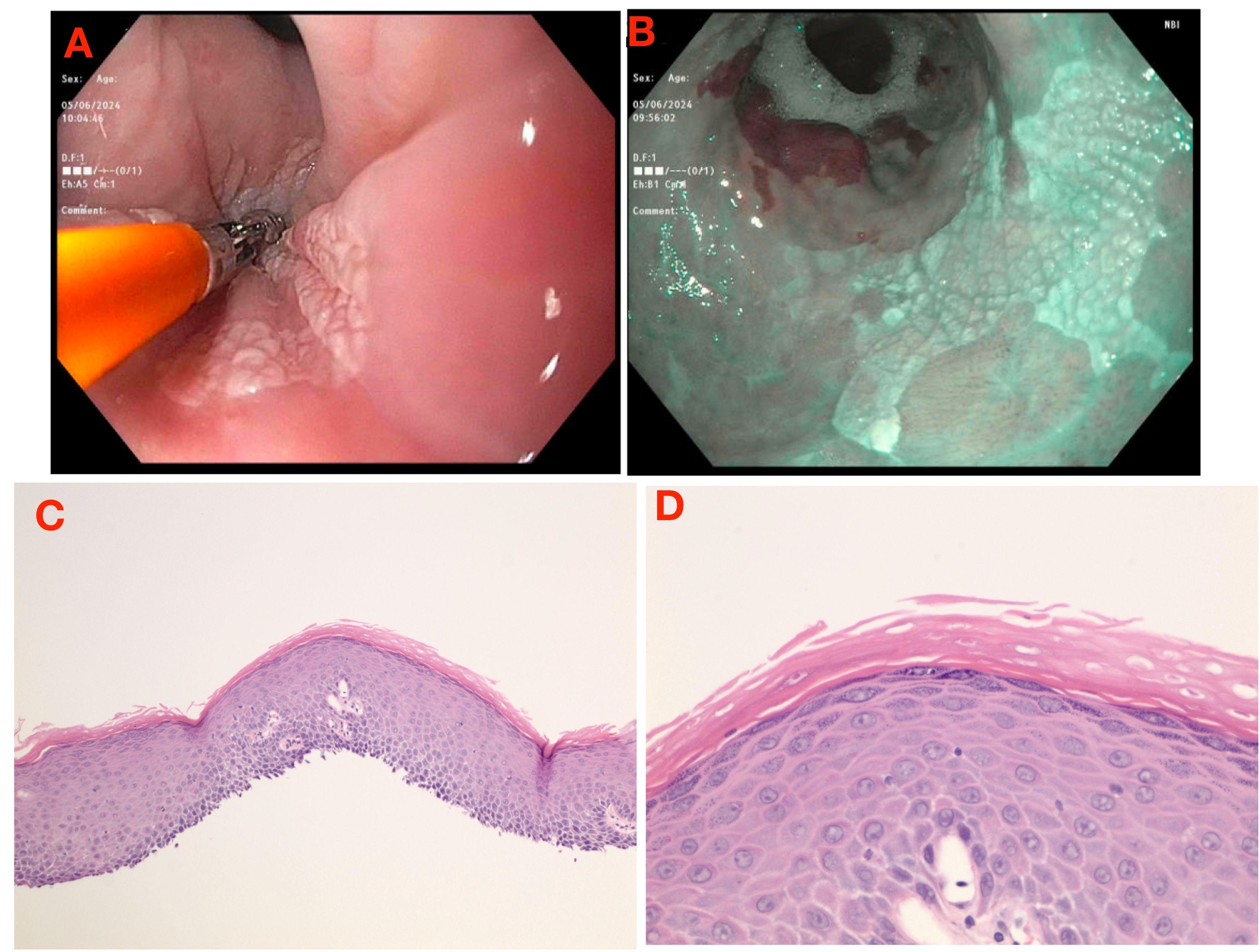
Introduction: Esophageal epidermoid metaplasia (EEM) is a rare condition that can lead to transformation into carcinoma. Endoscopic features of EEM vary with features including plaques, keratotic patches, or lacy appearance. Pathology usually confirms the diagnosis with hyperorthokeratosis and prominent granular cell layers. Due to its rarity it is often under-recognized with some cases not diagnosed until months later. While most patients have symptoms such as dysphagia prior to presentation, we report a patient without any symptoms who presented with a case of EEM.
Case Description/Methods: A 76 year old man with history significant for prostate cancer and family history of gastric cancer in his mother and two brothers initially presented for endoscopy secondary to his family history. On initial endoscopy he was found to have LA Grade A reflux esophagitis and a hyperplastic polyp. On follow up surveillance endoscopy three years later he was noted to have localized mild mucosal changes characterized by granularity and altered texture in the lower third of the esophagus. Notably he did not have any symptoms of reflux or dysphagia prior or after surveillance. Biopsy demonstrated esophageal epidermoid metaplasia with a separate fragment of squamous mucosa showing active neutrophilic esophagitis. He was subsequently referred for cryotherapy ablation.
Discussion: EEM is rare and has an association with esophageal squamous dysplasia and carcinoma. The largest case series of patients from 2021 analyzed 40 cases with EEM and demonstrated that ⅔ of these patients have dysphagia at time of their EEM diagnosis which precipitated EGD. Other cases were observed in the setting of SCC surveillance, BE surveillance, and GERD. 10% of cases had squamous neoplasia occurring prior, with, or after EEM diagnosis in comparison to 6.1% and 2.7% among patients with esophageal lichen planus and achalasia, highlighting a potential elevated risk. EEM is often hard to diagnose endoscopically but histology is crucial in diagnosis. Management involves ablation or endoscopic mucosal resection for easily resectable lesions and for larger lesions surveillance EGD with 4-quadrant biopsies every 6 months with subsequent annual EGD if no dysplasia or progression is noted. There are no consensus guidelines regarding surveillance endoscopy but with increasing recognition of EEM larger studies to examine outcomes and determine appropriate guidelines will be warranted.
Disclosures:
Suvithan Rajadurai, MD1, Syed Quadri, MD2, Daniel Greenwald, MD3, Samir Shah, MD3. P3979 - A Silent Risk: a Case of Esophageal Epidermoid Metaplasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Brown University / Rhode Island Hospital, Providence, RI; 2Brown Medicine/Lifespan, Providence, RI; 3Gastroenterology Associates, Providence, RI
Introduction: Esophageal epidermoid metaplasia (EEM) is a rare condition that can lead to transformation into carcinoma. Endoscopic features of EEM vary with features including plaques, keratotic patches, or lacy appearance. Pathology usually confirms the diagnosis with hyperorthokeratosis and prominent granular cell layers. Due to its rarity it is often under-recognized with some cases not diagnosed until months later. While most patients have symptoms such as dysphagia prior to presentation, we report a patient without any symptoms who presented with a case of EEM.
Case Description/Methods: A 76 year old man with history significant for prostate cancer and family history of gastric cancer in his mother and two brothers initially presented for endoscopy secondary to his family history. On initial endoscopy he was found to have LA Grade A reflux esophagitis and a hyperplastic polyp. On follow up surveillance endoscopy three years later he was noted to have localized mild mucosal changes characterized by granularity and altered texture in the lower third of the esophagus. Notably he did not have any symptoms of reflux or dysphagia prior or after surveillance. Biopsy demonstrated esophageal epidermoid metaplasia with a separate fragment of squamous mucosa showing active neutrophilic esophagitis. He was subsequently referred for cryotherapy ablation.
Discussion: EEM is rare and has an association with esophageal squamous dysplasia and carcinoma. The largest case series of patients from 2021 analyzed 40 cases with EEM and demonstrated that ⅔ of these patients have dysphagia at time of their EEM diagnosis which precipitated EGD. Other cases were observed in the setting of SCC surveillance, BE surveillance, and GERD. 10% of cases had squamous neoplasia occurring prior, with, or after EEM diagnosis in comparison to 6.1% and 2.7% among patients with esophageal lichen planus and achalasia, highlighting a potential elevated risk. EEM is often hard to diagnose endoscopically but histology is crucial in diagnosis. Management involves ablation or endoscopic mucosal resection for easily resectable lesions and for larger lesions surveillance EGD with 4-quadrant biopsies every 6 months with subsequent annual EGD if no dysplasia or progression is noted. There are no consensus guidelines regarding surveillance endoscopy but with increasing recognition of EEM larger studies to examine outcomes and determine appropriate guidelines will be warranted.
Figure: A-B.) Localized mild mucosal changes characterized by granularity and altered texture in the lower third of the esophagus under HD as well as narrow band imaging C-D.) Esophageal squamous epithelium with a prominent granular layer with keratohyalin granules resembling epidermis of skin
Disclosures:
Suvithan Rajadurai indicated no relevant financial relationships.
Syed Quadri indicated no relevant financial relationships.
Daniel Greenwald indicated no relevant financial relationships.
Samir Shah: Roche Information Systems – Consultant.
Suvithan Rajadurai, MD1, Syed Quadri, MD2, Daniel Greenwald, MD3, Samir Shah, MD3. P3979 - A Silent Risk: a Case of Esophageal Epidermoid Metaplasia, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
