Tuesday Poster Session
Category: Esophagus
P3980 - From Bad to Worse: Isolated Severe Esophageal Lichen Planus, Treated With Tacrolimus, Complicated by Esophageal Perforation
Tuesday, October 29, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Dauris D. Rosario Lora, MD
Rush University Medical Center
Chicago, IL
Presenting Author(s)
Dauris D. Rosario Lora, MD, Ummesalmah Abdulbaseer, MD, Caroline Wang, MD, Michael Brown, MD, MACM
Rush University Medical Center, Chicago, IL
Introduction: Esophageal Lichen Planus (ELP) is a poorly understood inflammatory condition primarily presenting as odynophagia and/or dysphagia. Diagnostic challenges arise from endoscopic findings resembling other disorders, and by non-specific pathology results. Treatment typically involves corticosteroids and immunosuppressants.1 Here, we report a case of severe ELP where the interplay between the disease and treatment resulted in esophageal perforation.
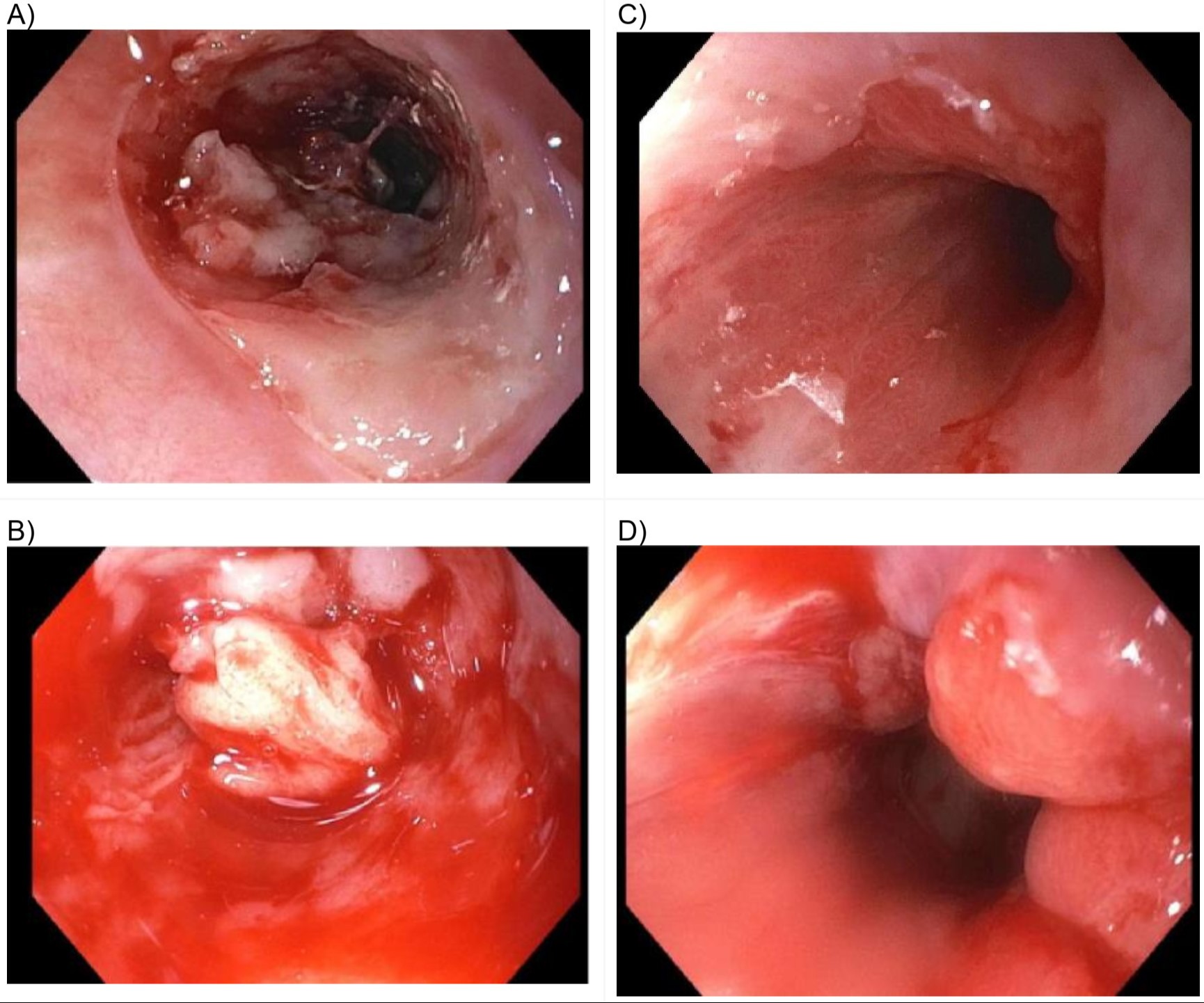
Case Description/Methods: A 78-year-old, presented to clinic with dysphagia to both solids and liquids. Initial
esophagogastroduodenoscopy (EGD) demonstrated severe esophagitis and mucosal sloughing,
initially thought to be Esophagitis Dissecans Superficialis (EDS), with his biopsy showing necrotic
exudate with inflammatory granulation tissue and negative viral staining. Extensive workup,
including swallowing, and motility testing, were unremarkable. Oral and IV steroids demonstrated
minimal response. The patient required multiple EGDs with dilations and steroid injections to have
any oral intake. Multiple biopsies were negative for viral staining and immunofluorescence (Figure
1). A diagnosis of esophageal lichen planus was felt to be most consistent with his refractory
clinical course. He was eventually started on topical tacrolimus 0.1% swish and swallow, leading
to an almost complete clinical and endoscopic remission after 4 months of treatment (Figure 2).
Unfortunately, the patient suffered a spontaneous esophageal perforation, requiring
esophagectomy 6 months after starting oral tacrolimus.
Discussion: Esophageal lichen planus is an often-overlooked diagnosis. Typically, the appearance of EDS is similar to ELP2. Absent pathological confirmation should not exclude the diagnosis of ELP4. ELP is often treated with steroids, but if they are unable to provide proper symptomatic control, then dilation and immunosuppressive drugs are the appropriate next steps5,6. This patient’s need for multiple dilations and positive response to oral tacrolimus is very suggestive of biopsy-negative ELP. Although his subsequent esophageal perforation could have been sequelae of ELP itself, it could also be the result of tacrolimus toxicity, which has been reported to cause gastrointestinal side effects like nausea, diarrhea1, esophageal and colonic ulceration10, and acute esophageal necrosis11. This case highlights both the efficacy and danger of using tacrolimus as a treatment for ELP refractory to steroids.
Disclosures:
Dauris D. Rosario Lora, MD, Ummesalmah Abdulbaseer, MD, Caroline Wang, MD, Michael Brown, MD, MACM. P3980 - From Bad to Worse: Isolated Severe Esophageal Lichen Planus, Treated With Tacrolimus, Complicated by Esophageal Perforation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Rush University Medical Center, Chicago, IL
Introduction: Esophageal Lichen Planus (ELP) is a poorly understood inflammatory condition primarily presenting as odynophagia and/or dysphagia. Diagnostic challenges arise from endoscopic findings resembling other disorders, and by non-specific pathology results. Treatment typically involves corticosteroids and immunosuppressants.1 Here, we report a case of severe ELP where the interplay between the disease and treatment resulted in esophageal perforation.
Case Description/Methods: A 78-year-old, presented to clinic with dysphagia to both solids and liquids. Initial
esophagogastroduodenoscopy (EGD) demonstrated severe esophagitis and mucosal sloughing,
initially thought to be Esophagitis Dissecans Superficialis (EDS), with his biopsy showing necrotic
exudate with inflammatory granulation tissue and negative viral staining. Extensive workup,
including swallowing, and motility testing, were unremarkable. Oral and IV steroids demonstrated
minimal response. The patient required multiple EGDs with dilations and steroid injections to have
any oral intake. Multiple biopsies were negative for viral staining and immunofluorescence (Figure
1). A diagnosis of esophageal lichen planus was felt to be most consistent with his refractory
clinical course. He was eventually started on topical tacrolimus 0.1% swish and swallow, leading
to an almost complete clinical and endoscopic remission after 4 months of treatment (Figure 2).
Unfortunately, the patient suffered a spontaneous esophageal perforation, requiring
esophagectomy 6 months after starting oral tacrolimus.
Discussion: Esophageal lichen planus is an often-overlooked diagnosis. Typically, the appearance of EDS is similar to ELP2. Absent pathological confirmation should not exclude the diagnosis of ELP4. ELP is often treated with steroids, but if they are unable to provide proper symptomatic control, then dilation and immunosuppressive drugs are the appropriate next steps5,6. This patient’s need for multiple dilations and positive response to oral tacrolimus is very suggestive of biopsy-negative ELP. Although his subsequent esophageal perforation could have been sequelae of ELP itself, it could also be the result of tacrolimus toxicity, which has been reported to cause gastrointestinal side effects like nausea, diarrhea1, esophageal and colonic ulceration10, and acute esophageal necrosis11. This case highlights both the efficacy and danger of using tacrolimus as a treatment for ELP refractory to steroids.
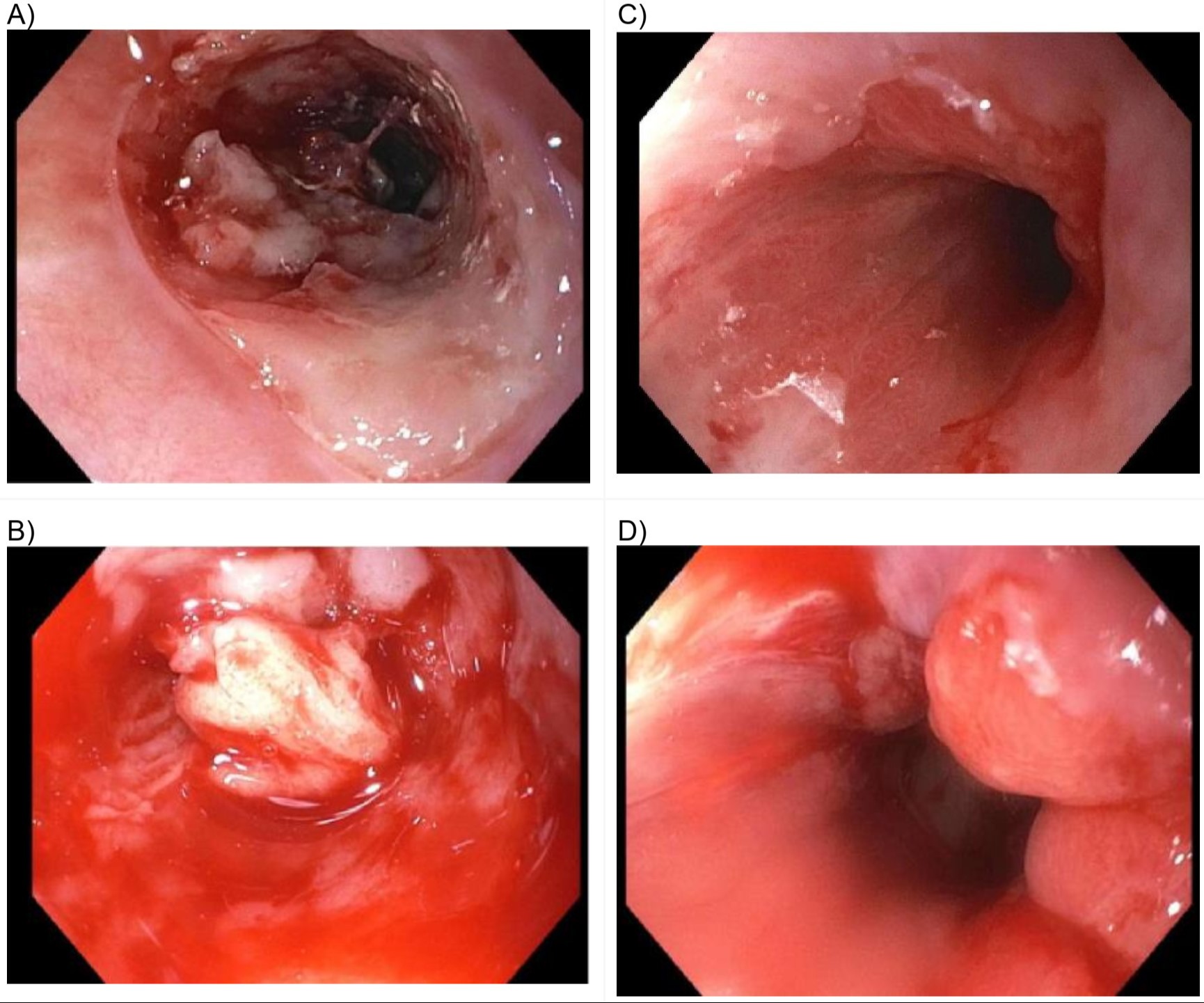
Figure: Figure 1, Endoscopic imaging before and after tacrolimus treatment initiated. Pictures on the left (A, B), show findings of severe esophagitis, sloughing mucosa, and stenosis, seen on EGDs prior to starting tacrolimus treatment. Pictures on the right (C, D) show improvement of stenosis, as well as less inflammatory changes on the lower third of the esophagus after 4 months of tacrolimus treatment.
Disclosures:
Dauris Rosario Lora indicated no relevant financial relationships.
Ummesalmah Abdulbaseer indicated no relevant financial relationships.
Caroline Wang indicated no relevant financial relationships.
Michael Brown indicated no relevant financial relationships.
Dauris D. Rosario Lora, MD, Ummesalmah Abdulbaseer, MD, Caroline Wang, MD, Michael Brown, MD, MACM. P3980 - From Bad to Worse: Isolated Severe Esophageal Lichen Planus, Treated With Tacrolimus, Complicated by Esophageal Perforation, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
