Monday Poster Session
Category: Liver
P2910 - Ketamine-Induced Cholangiopathy: A Case Series
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- CW
Carolyn Wilson, BA, MD
NYU Langone Health
New York, NY
Presenting Author(s)
Carolyn Wilson, BA, MD, Katie Shen, BS, MD, Saikiran Kilaru, MD
NYU Langone Health, New York, NY
Introduction: Ketamine is a N-methyl-D-aspartate (NMDA) receptor antagonist widely utilized for its concurrent analgesic and anesthetic properties, but it is also used recreationally for its hallucinogenic and dissociative assets. There is a predominance of use in East and South-East Asia, with rates of ketamine users in Hong Kong increasing from 9.8% of total drug users in 2000 to 37.6% in 2009. Known consequences of ketamine misuse include ulcerative cystitis and neurocognitive impairment, but cholangiopathy is not well studied. FDA-approved use of esketamine for depression may cause increased relevance for gastroenterologists in the future.
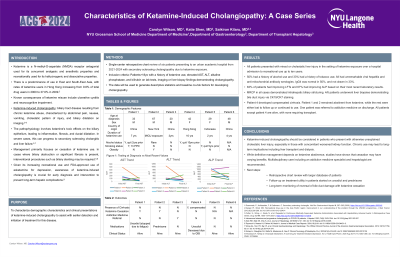
Methods: We performed a retrospective review of six patients presenting to an urban academic hospital from 2021-2024 with secondary sclerosing cholangiopathy due to ketamine exposure. Demographic data was collected regarding patients’ clinical characteristics, labs and imaging at time of diagnosis, and patient outcomes.
Results: All patients presented with mixed or cholestatic liver injury in the setting of ketamine exposure over a hospital admission to recreational use up to ten years. 50% had a history of alcohol use and 33% had a history of tobacco use. All had unremarkable viral hepatitis and anti-mitochondrial antibody serologies. IgG4 was normal in 50%, and not drawn in 2/6. MRCP in all cases demonstrated intrahepatic biliary stricturing. 4/6 patients underwent liver biopsies demonstrating bile duct injury via CK19/CK7 staining. Patient 4 developed compensated cirrhosis. Patient 1 remained abstinent from ketamine, while the rest were either lost to follow up or continued to use. One patient was referred to addiction medicine on discharge. All patients except patient 4 are alive, with none requiring transplant. Two were started on ursodiol, and one was started on prednisone.
Discussion: Ketamine-induced cholangiopathy should be considered in patients who present with otherwise unexplained cholestatic liver injury, especially in those with concomitant worsened kidney function. Chronic use may be associated with bile duct inflammation and fibrosis resulting in strictures and hepatocyte injury, leading to long-term implications including liver transplant and dialysis. While definitive management depends on ketamine abstinence, studies have shown that stricturing disease may be permanent and cessation may have varying benefits. Multidisciplinary care including an addiction medicine specialist and hepatologist may be useful to assist with abstinence.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Carolyn Wilson, BA, MD, Katie Shen, BS, MD, Saikiran Kilaru, MD. P2910 - Ketamine-Induced Cholangiopathy: A Case Series, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
NYU Langone Health, New York, NY
Introduction: Ketamine is a N-methyl-D-aspartate (NMDA) receptor antagonist widely utilized for its concurrent analgesic and anesthetic properties, but it is also used recreationally for its hallucinogenic and dissociative assets. There is a predominance of use in East and South-East Asia, with rates of ketamine users in Hong Kong increasing from 9.8% of total drug users in 2000 to 37.6% in 2009. Known consequences of ketamine misuse include ulcerative cystitis and neurocognitive impairment, but cholangiopathy is not well studied. FDA-approved use of esketamine for depression may cause increased relevance for gastroenterologists in the future.
Methods: We performed a retrospective review of six patients presenting to an urban academic hospital from 2021-2024 with secondary sclerosing cholangiopathy due to ketamine exposure. Demographic data was collected regarding patients’ clinical characteristics, labs and imaging at time of diagnosis, and patient outcomes.
Results: All patients presented with mixed or cholestatic liver injury in the setting of ketamine exposure over a hospital admission to recreational use up to ten years. 50% had a history of alcohol use and 33% had a history of tobacco use. All had unremarkable viral hepatitis and anti-mitochondrial antibody serologies. IgG4 was normal in 50%, and not drawn in 2/6. MRCP in all cases demonstrated intrahepatic biliary stricturing. 4/6 patients underwent liver biopsies demonstrating bile duct injury via CK19/CK7 staining. Patient 4 developed compensated cirrhosis. Patient 1 remained abstinent from ketamine, while the rest were either lost to follow up or continued to use. One patient was referred to addiction medicine on discharge. All patients except patient 4 are alive, with none requiring transplant. Two were started on ursodiol, and one was started on prednisone.
Discussion: Ketamine-induced cholangiopathy should be considered in patients who present with otherwise unexplained cholestatic liver injury, especially in those with concomitant worsened kidney function. Chronic use may be associated with bile duct inflammation and fibrosis resulting in strictures and hepatocyte injury, leading to long-term implications including liver transplant and dialysis. While definitive management depends on ketamine abstinence, studies have shown that stricturing disease may be permanent and cessation may have varying benefits. Multidisciplinary care including an addiction medicine specialist and hepatologist may be useful to assist with abstinence.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Carolyn Wilson indicated no relevant financial relationships.
Katie Shen indicated no relevant financial relationships.
Saikiran Kilaru indicated no relevant financial relationships.
Carolyn Wilson, BA, MD, Katie Shen, BS, MD, Saikiran Kilaru, MD. P2910 - Ketamine-Induced Cholangiopathy: A Case Series, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

