Monday Poster Session
Category: Liver
P2915 - Hepatitis See You Later: Faster Time-to-Treatment of Chronic Hepatitis C in an Addiction Medicine Clinic
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
.jpg)
James F. Burton, MD
University of Iowa Health Care
Iowa City, IA
Presenting Author(s)
James F. Burton, MD1, Lakshmi Guduguntla, MD1, Marcus Osman, MD1, Joseph Rattenni, DO2, Arya Zandvakili, MD, PhD1, Sayeh Sabbagh, BA1, Stephan Arndt, PhD3, Alison Lynch, MD1, Andrea Weber, MD1
1University of Iowa Health Care, Iowa City, IA; 2University of Iowa Health Care, Tiffin, IA; 3University of Iowa Health Care, Coralville, IA
Introduction: There has been a substantial increase in chronic hepatitis C virus (HCV) infections among people with substance use disorders (SUD). In 2020, these authors’ state Medicaid lifted restrictions on HCV treatment, allowing for treatment of HCV without an Infectious Disease or Hepatology prescriber requirement. As a result, our local addiction medicine (AM) clinic sought to create an interdisciplinary care model to expedite screening and treatment of HCV in a predominantly rural state. We aimed to assess if integrating HCV care into an AM clinic improved efficiency of HCV treatment.
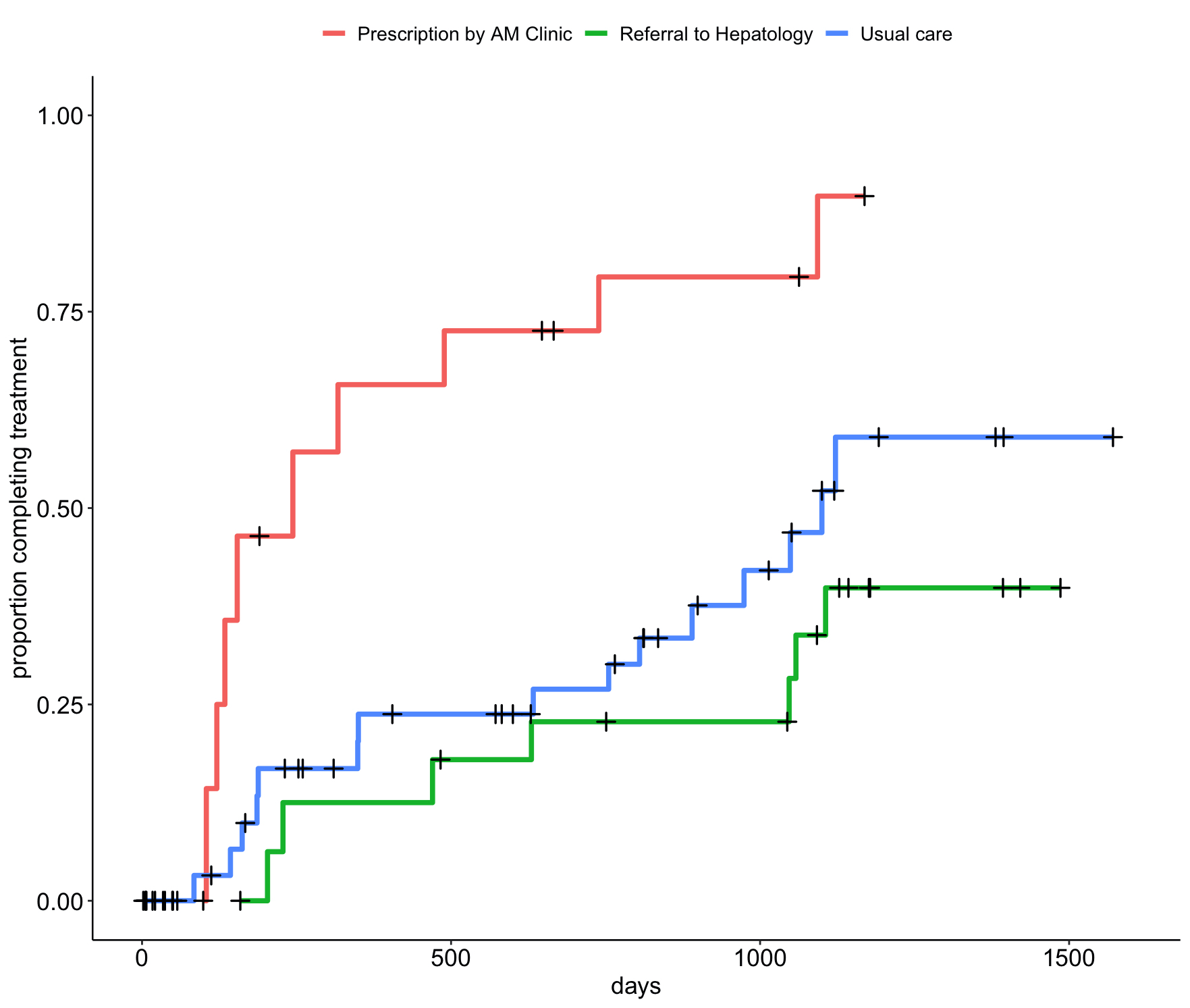
Methods: We performed a retrospective chart review of patients seen in an AM clinic between 01/01/2019 and 05/31/2023. We assessed three forms of care for HCV 1) prescription by AM clinic, 2) referral to Hepatology clinic for treatment, and 3) usual care, defined by those not included in groups 1 or 2. Our primary endpoint was time-to-completion of antiviral therapy or negative HCV viral load. Statistical analysis was performed using a Cox proportional hazard model, with the three forms of care incorporated as a time-dependent covariate (usual care as a control).
Results: We identified 80 patients as having chronic HCV while attending AM clinic within the study period. Thirty percent of the cohort was Female, 87% was White, and median age upon entry was 34 years. After the state Medicaid policy was relaxed, 9 out of 15 patients completed treatment when prescribed an antiviral by AM clinic, 7 out of 22 patients completed treatment when referred to Hepatology, and 15 out of 56 patients completed treatment with usual care. Receiving an antiviral prescription from AM clinic was associated with a faster time-to-treatment compared to usual care (hazard ratio [HR]: 5.0; 95% confidence interval [CI]: 1.9-12). In contrast, patients referred to Hepatology for treatment did not have a faster time-to-treatment compared to usual care (HR 0.94; 95% CI 0.44-1.97). These results are indicated in Figure 1.
Discussion: Management of chronic HCV in an AM clinic was associated with a faster time-to-treatment of HCV compared to usual care. There was no difference in time-to-treatment of HCV between Hepatology referral and usual care. These results may inform how policy changes and integration of HCV care into AM clinics can lead to a reduced public health burden of HCV.
Disclosures:
James F. Burton, MD1, Lakshmi Guduguntla, MD1, Marcus Osman, MD1, Joseph Rattenni, DO2, Arya Zandvakili, MD, PhD1, Sayeh Sabbagh, BA1, Stephan Arndt, PhD3, Alison Lynch, MD1, Andrea Weber, MD1. P2915 - Hepatitis See You Later: Faster Time-to-Treatment of Chronic Hepatitis C in an Addiction Medicine Clinic, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Iowa Health Care, Iowa City, IA; 2University of Iowa Health Care, Tiffin, IA; 3University of Iowa Health Care, Coralville, IA
Introduction: There has been a substantial increase in chronic hepatitis C virus (HCV) infections among people with substance use disorders (SUD). In 2020, these authors’ state Medicaid lifted restrictions on HCV treatment, allowing for treatment of HCV without an Infectious Disease or Hepatology prescriber requirement. As a result, our local addiction medicine (AM) clinic sought to create an interdisciplinary care model to expedite screening and treatment of HCV in a predominantly rural state. We aimed to assess if integrating HCV care into an AM clinic improved efficiency of HCV treatment.
Methods: We performed a retrospective chart review of patients seen in an AM clinic between 01/01/2019 and 05/31/2023. We assessed three forms of care for HCV 1) prescription by AM clinic, 2) referral to Hepatology clinic for treatment, and 3) usual care, defined by those not included in groups 1 or 2. Our primary endpoint was time-to-completion of antiviral therapy or negative HCV viral load. Statistical analysis was performed using a Cox proportional hazard model, with the three forms of care incorporated as a time-dependent covariate (usual care as a control).
Results: We identified 80 patients as having chronic HCV while attending AM clinic within the study period. Thirty percent of the cohort was Female, 87% was White, and median age upon entry was 34 years. After the state Medicaid policy was relaxed, 9 out of 15 patients completed treatment when prescribed an antiviral by AM clinic, 7 out of 22 patients completed treatment when referred to Hepatology, and 15 out of 56 patients completed treatment with usual care. Receiving an antiviral prescription from AM clinic was associated with a faster time-to-treatment compared to usual care (hazard ratio [HR]: 5.0; 95% confidence interval [CI]: 1.9-12). In contrast, patients referred to Hepatology for treatment did not have a faster time-to-treatment compared to usual care (HR 0.94; 95% CI 0.44-1.97). These results are indicated in Figure 1.
Discussion: Management of chronic HCV in an AM clinic was associated with a faster time-to-treatment of HCV compared to usual care. There was no difference in time-to-treatment of HCV between Hepatology referral and usual care. These results may inform how policy changes and integration of HCV care into AM clinics can lead to a reduced public health burden of HCV.
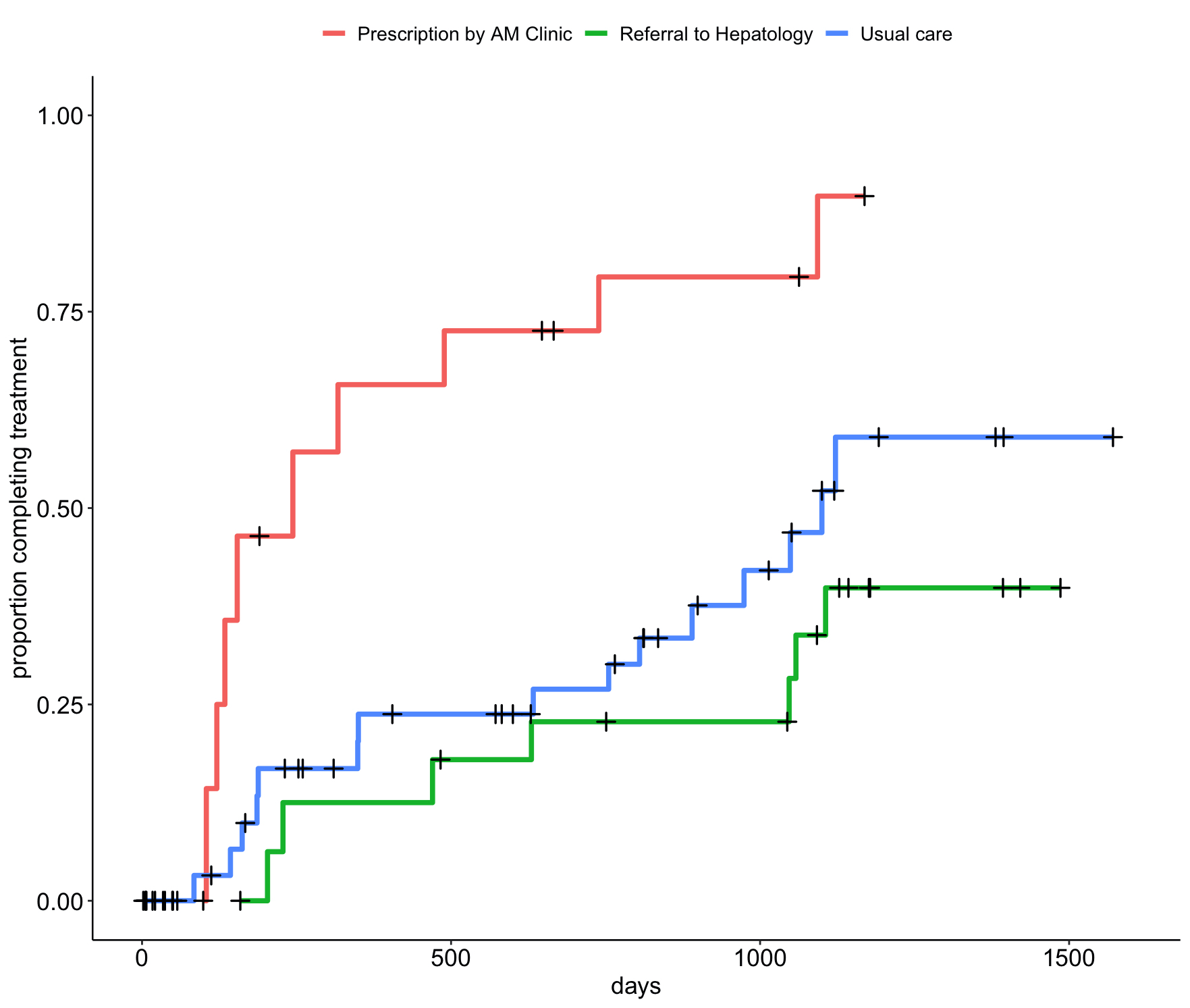
Figure: Figure 1. Time-to-Treatment of Antiviral Therapy
Disclosures:
James Burton indicated no relevant financial relationships.
Lakshmi Guduguntla indicated no relevant financial relationships.
Marcus Osman indicated no relevant financial relationships.
Joseph Rattenni indicated no relevant financial relationships.
Arya Zandvakili indicated no relevant financial relationships.
Sayeh Sabbagh indicated no relevant financial relationships.
Stephan Arndt indicated no relevant financial relationships.
Alison Lynch indicated no relevant financial relationships.
Andrea Weber indicated no relevant financial relationships.
James F. Burton, MD1, Lakshmi Guduguntla, MD1, Marcus Osman, MD1, Joseph Rattenni, DO2, Arya Zandvakili, MD, PhD1, Sayeh Sabbagh, BA1, Stephan Arndt, PhD3, Alison Lynch, MD1, Andrea Weber, MD1. P2915 - Hepatitis See You Later: Faster Time-to-Treatment of Chronic Hepatitis C in an Addiction Medicine Clinic, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

