Monday Poster Session
Category: Liver
P2920 - Fecal Microbiota Transplantation: A Potential Game Changer for Severe Alcoholic Hepatitis? A Systematic Review and Meta-Analysis.
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- MH
Mahmoud A. Hashim, MD
SBH Health System
New Rochelle, NY
Presenting Author(s)
Mahmoud A.. Hashim, MD1, Mohamed Awad, MD2, Mohamed Seisa, MD3, Ahmed M. Afifi, MBBCh4, Ahmed S.. ELgammal, MD, MS5, Waliullah khan, MD6, Irma Lorena G. Langlois Zepeda, MD7, Mahmoud M. Ali, MD8, Ranya Selim, MD9
1SBH Health System, New Rochelle, NY; 2Ain Shams University, Cairo, Al Qahirah, Egypt; 3UNC Health Blue Ridge, Morganton, NC; 4University of Toledo College Medicine and Life Sciences, Toledo, OH; 5Dar El-Shefa Hospital, Cairo, Al Qahirah, Egypt; 6Cairo University, Dearborn, MI; 7SBH Health System, Bronx, NY; 8SBH Health System, Ridgefield, NJ; 9University of Texas at Houston, Houston, TX
Introduction: Severe alcoholic hepatitis (SAH) is a significant public health concern in the United States, with a 28-day mortality rate of 30-50%. Available medical therapies, namely steroids and pentoxifylline have failed to demonstrate large-scale consistent, significant improvement in long-term survival. Emerging evidence suggests that gut-derived bacterial endotoxins contribute to alcohol-induced liver injury, and fecal microbiota transplantation (FMT) may offer a potential treatment for SAH.
Methods: PubMed, Web of Science, Scopus, Embase and Cochrane databases were queried through May 2024, to identify studies comparing efficacy and safety of FMT and standard of care in SAH patients. The search generated 1055 studies, of which duplicates, animal studies, case reports, conference abstracts and otherwise irrelevant manuscripts were excluded. Meta-analysis was performed using Open-Meta Analyst to estimate pooled relative risk (RR), 95% confidence interval (95%CI) and heterogeneity (I2).
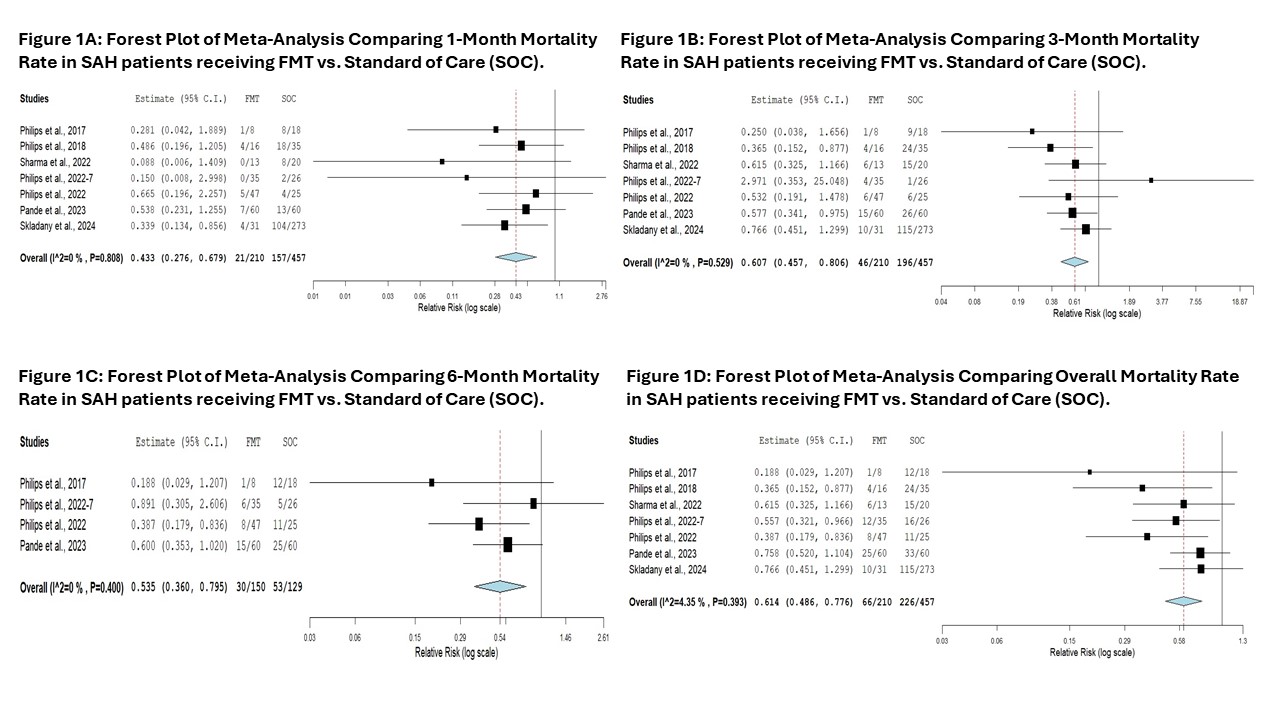
Results: A total of seven studies out of 704 screened were included. Study baseline characteristics are described in table 1. Our analysis revealed that patients receiving FMT had a significantly lower risk of mortality at 1, 3, and 6 months, as well as overall mortality, compared to those receiving standard of care (SOC) [Figure 1]. Additionally, patients who received FMT were more likely to experience resolution of ascites (RR =2.06, 95% CI: 0.95 -3.43) and hepatic encephalopathy (RR =1.71, 95% CI: 1.03 -2.85) compared to those receiving SOC. Furthermore, the FMT group was less likely to develop acute kidney injury (RR =0.63, 95% CI: 0.42 -0.96), variceal bleeding (RR =0.82, 95% CI: 0.51 -1.33) and spontaneous bacterial peritonitis (RR =0.55, 95% CI: 0.186 -1.64).
Discussion: These findings demonstrate a trend towards improvement in both short- and long-term survival in patients receiving FMT, suggesting this may be an effective and safe therapy for SAH. However, due to the small number of patients in each study and the studies predominantly being from India, further large-scale controlled studies are warranted to confirm these results and expand their generalizability.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mahmoud A.. Hashim, MD1, Mohamed Awad, MD2, Mohamed Seisa, MD3, Ahmed M. Afifi, MBBCh4, Ahmed S.. ELgammal, MD, MS5, Waliullah khan, MD6, Irma Lorena G. Langlois Zepeda, MD7, Mahmoud M. Ali, MD8, Ranya Selim, MD9. P2920 - Fecal Microbiota Transplantation: A Potential Game Changer for Severe Alcoholic Hepatitis? A Systematic Review and Meta-Analysis., ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1SBH Health System, New Rochelle, NY; 2Ain Shams University, Cairo, Al Qahirah, Egypt; 3UNC Health Blue Ridge, Morganton, NC; 4University of Toledo College Medicine and Life Sciences, Toledo, OH; 5Dar El-Shefa Hospital, Cairo, Al Qahirah, Egypt; 6Cairo University, Dearborn, MI; 7SBH Health System, Bronx, NY; 8SBH Health System, Ridgefield, NJ; 9University of Texas at Houston, Houston, TX
Introduction: Severe alcoholic hepatitis (SAH) is a significant public health concern in the United States, with a 28-day mortality rate of 30-50%. Available medical therapies, namely steroids and pentoxifylline have failed to demonstrate large-scale consistent, significant improvement in long-term survival. Emerging evidence suggests that gut-derived bacterial endotoxins contribute to alcohol-induced liver injury, and fecal microbiota transplantation (FMT) may offer a potential treatment for SAH.
Methods: PubMed, Web of Science, Scopus, Embase and Cochrane databases were queried through May 2024, to identify studies comparing efficacy and safety of FMT and standard of care in SAH patients. The search generated 1055 studies, of which duplicates, animal studies, case reports, conference abstracts and otherwise irrelevant manuscripts were excluded. Meta-analysis was performed using Open-Meta Analyst to estimate pooled relative risk (RR), 95% confidence interval (95%CI) and heterogeneity (I2).
Results: A total of seven studies out of 704 screened were included. Study baseline characteristics are described in table 1. Our analysis revealed that patients receiving FMT had a significantly lower risk of mortality at 1, 3, and 6 months, as well as overall mortality, compared to those receiving standard of care (SOC) [Figure 1]. Additionally, patients who received FMT were more likely to experience resolution of ascites (RR =2.06, 95% CI: 0.95 -3.43) and hepatic encephalopathy (RR =1.71, 95% CI: 1.03 -2.85) compared to those receiving SOC. Furthermore, the FMT group was less likely to develop acute kidney injury (RR =0.63, 95% CI: 0.42 -0.96), variceal bleeding (RR =0.82, 95% CI: 0.51 -1.33) and spontaneous bacterial peritonitis (RR =0.55, 95% CI: 0.186 -1.64).
Discussion: These findings demonstrate a trend towards improvement in both short- and long-term survival in patients receiving FMT, suggesting this may be an effective and safe therapy for SAH. However, due to the small number of patients in each study and the studies predominantly being from India, further large-scale controlled studies are warranted to confirm these results and expand their generalizability.
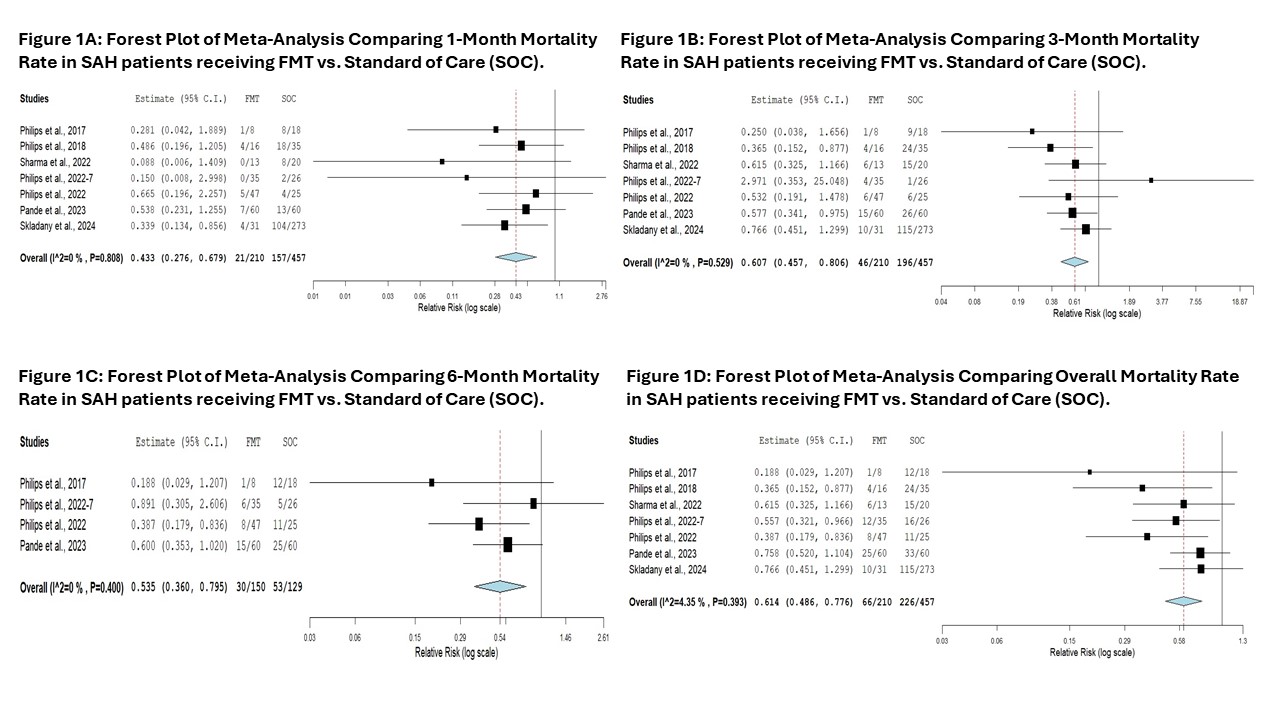
Figure: Figure 1: Forest Plots of Meta-Analysis Comparing Mortality Rates in SAH patients receiving FMT vs. Standard of Care (SOC).
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Mahmoud Hashim indicated no relevant financial relationships.
Mohamed Awad indicated no relevant financial relationships.
Mohamed Seisa indicated no relevant financial relationships.
Ahmed M. Afifi indicated no relevant financial relationships.
Ahmed ELgammal indicated no relevant financial relationships.
Waliullah khan indicated no relevant financial relationships.
Irma Lorena Langlois Zepeda indicated no relevant financial relationships.
Mahmoud Ali indicated no relevant financial relationships.
Ranya Selim indicated no relevant financial relationships.
Mahmoud A.. Hashim, MD1, Mohamed Awad, MD2, Mohamed Seisa, MD3, Ahmed M. Afifi, MBBCh4, Ahmed S.. ELgammal, MD, MS5, Waliullah khan, MD6, Irma Lorena G. Langlois Zepeda, MD7, Mahmoud M. Ali, MD8, Ranya Selim, MD9. P2920 - Fecal Microbiota Transplantation: A Potential Game Changer for Severe Alcoholic Hepatitis? A Systematic Review and Meta-Analysis., ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
