Monday Poster Session
Category: Liver
P2925 - The Incidence of Spontaneous Bacterial Peritonitis in Decompensated Cirrhotics With Gastric Antral Vascular Ectasia and Associated Risk Factors
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Atul Lodh, MD
University of Alabama at Birmingham Heersink School of Medicine
Birmingham, AL
Presenting Author(s)
Thomas Ruli, MD1, Mahmoud Aryan, MD2, Atul Lodh, MD2, Mohamed Shoreibah, MD3, Shajan Peter, MD4
1University of Alabama at Birmingham, Birmingham, AL; 2University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 3University of Alabama at Birmingham Hospital, Birmingham, AL; 4Basil I. Hirschowitz Endoscopic Center of Excellence, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
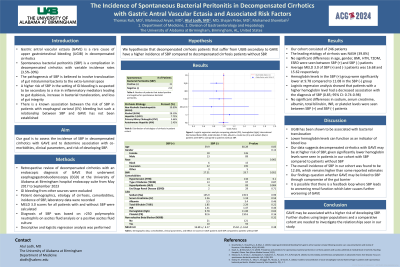
Introduction: Gastric antral vascular ectasia (GAVE) is a rare cause of upper gastrointestinal bleeding (UGIB) in decompensated cirrhotics (DCs). Spontaneous bacterial peritonitis (SBP) is a complication in DCs with variable incidence rates (3.5%-30%). Our goal is to assess the incidence of SBP in DCs with GAVE and determine association with comorbidities and risk of developing SBP.
Methods: We performed a retrospective review of DCs with an endoscopic diagnosis of GAVE that underwent an esophagogastroduodenoscopy (EGD) at our institution’s hospital endoscopy suite from May 2017 - September 2023. Those with UGIB from other sources were excluded. Patient demographics, etiology of cirrhosis, comorbidities, incidence of SBP, renal function, and hemoglobin levels were recorded. SBP diagnosis was based on >250 polymorphic neutrophils on ascites fluid analysis, a positive ascites fluid culture or prior history of SBP in which the patient was on prophylactic antibiotics. A logistic regression analysis was performed.
Results: Our cohort included 246 patients; average age was 60.66±10.60 years and BMI 30.04±6.77. 56.5% were male and 88.2% were white. The leading etiology of cirrhosis was NASH (39.8%). Comorbidities included hypertension (60.6%), diabetes mellitus (45.1%), hyperlipidemia (38.2%), chronic kidney disease (CKD) (36.9%) and end stage renal disease (ESRD) (3.7%). Average hemoglobin was 11.55±5.45 with average MELD 3.0 of 15.62±6.64. Among our cohort, 31 (12.6%) had SBP. Among these, 14 had CKD (45.2%) and 2 had ESRD (6.5%); the average creatinine of these patients was 1.26±0.74 and the average hemoglobin was 9.78±2.96. A logistic regression analysis showed that patients with a higher hemoglobin level had decreased association with the diagnosis of SBP (OR 0.85; CI: 0.74-0.98; p=0.34).
Discussion: Our data suggests DCs with GAVE may be at higher risk of SBP given risk of chronic UGIB and renal disease when compared to other cirrhotic populations. The overall incidence of SBP in our cohort was found to be 12.6%, which remains higher than some reported estimates. Our findings question whether GAVE may be linked to SBP through a rise in inflammatory mediators leading to gut dysbiosis, loss of gut integrity, and subsequent bacterial translocation. It is possible that there is a feedback loop where SBP leads to worsening renal function which later causes further worsening of GAVE. Further studies using larger populations and a comparative cohort are needed to further investigate.
Disclosures:
Thomas Ruli, MD1, Mahmoud Aryan, MD2, Atul Lodh, MD2, Mohamed Shoreibah, MD3, Shajan Peter, MD4. P2925 - The Incidence of Spontaneous Bacterial Peritonitis in Decompensated Cirrhotics With Gastric Antral Vascular Ectasia and Associated Risk Factors, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Alabama at Birmingham, Birmingham, AL; 2University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL; 3University of Alabama at Birmingham Hospital, Birmingham, AL; 4Basil I. Hirschowitz Endoscopic Center of Excellence, The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
Introduction: Gastric antral vascular ectasia (GAVE) is a rare cause of upper gastrointestinal bleeding (UGIB) in decompensated cirrhotics (DCs). Spontaneous bacterial peritonitis (SBP) is a complication in DCs with variable incidence rates (3.5%-30%). Our goal is to assess the incidence of SBP in DCs with GAVE and determine association with comorbidities and risk of developing SBP.
Methods: We performed a retrospective review of DCs with an endoscopic diagnosis of GAVE that underwent an esophagogastroduodenoscopy (EGD) at our institution’s hospital endoscopy suite from May 2017 - September 2023. Those with UGIB from other sources were excluded. Patient demographics, etiology of cirrhosis, comorbidities, incidence of SBP, renal function, and hemoglobin levels were recorded. SBP diagnosis was based on >250 polymorphic neutrophils on ascites fluid analysis, a positive ascites fluid culture or prior history of SBP in which the patient was on prophylactic antibiotics. A logistic regression analysis was performed.
Results: Our cohort included 246 patients; average age was 60.66±10.60 years and BMI 30.04±6.77. 56.5% were male and 88.2% were white. The leading etiology of cirrhosis was NASH (39.8%). Comorbidities included hypertension (60.6%), diabetes mellitus (45.1%), hyperlipidemia (38.2%), chronic kidney disease (CKD) (36.9%) and end stage renal disease (ESRD) (3.7%). Average hemoglobin was 11.55±5.45 with average MELD 3.0 of 15.62±6.64. Among our cohort, 31 (12.6%) had SBP. Among these, 14 had CKD (45.2%) and 2 had ESRD (6.5%); the average creatinine of these patients was 1.26±0.74 and the average hemoglobin was 9.78±2.96. A logistic regression analysis showed that patients with a higher hemoglobin level had decreased association with the diagnosis of SBP (OR 0.85; CI: 0.74-0.98; p=0.34).
Discussion: Our data suggests DCs with GAVE may be at higher risk of SBP given risk of chronic UGIB and renal disease when compared to other cirrhotic populations. The overall incidence of SBP in our cohort was found to be 12.6%, which remains higher than some reported estimates. Our findings question whether GAVE may be linked to SBP through a rise in inflammatory mediators leading to gut dysbiosis, loss of gut integrity, and subsequent bacterial translocation. It is possible that there is a feedback loop where SBP leads to worsening renal function which later causes further worsening of GAVE. Further studies using larger populations and a comparative cohort are needed to further investigate.
Disclosures:
Thomas Ruli indicated no relevant financial relationships.
Mahmoud Aryan indicated no relevant financial relationships.
Atul Lodh indicated no relevant financial relationships.
Mohamed Shoreibah indicated no relevant financial relationships.
Shajan Peter: Olympus – Consultant.
Thomas Ruli, MD1, Mahmoud Aryan, MD2, Atul Lodh, MD2, Mohamed Shoreibah, MD3, Shajan Peter, MD4. P2925 - The Incidence of Spontaneous Bacterial Peritonitis in Decompensated Cirrhotics With Gastric Antral Vascular Ectasia and Associated Risk Factors, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

