Monday Poster Session
Category: Liver
P2930 - Evaluating Liver Transplant Referral Rates and Disparities Among Cirrhotic Patients: A Study in the Hispanic Population
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Shivangini Duggal, MD
TTUHSC
El Paso, TX
Presenting Author(s)
Shivangini Duggal, MD1, Bhavi Trivedi, MD2, Hedaia Algheriani, MD2, Michel Toutoungy, MD3, Li Guowei, MD4, Alejandro Robles, MD2, Sheldon Rao, MD2
1TTUHSC, El Paso, TX; 2Texas Tech University Health Sciences Center, El Paso, TX; 3Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, TX; 4Texas Tech University Health Sciences Center, EL Paso, TX
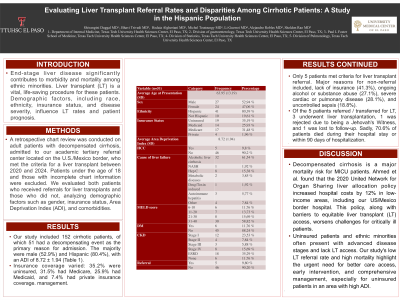
Introduction: End-stage liver disease significantly contributes to morbidity and mortality among ethnic minorities. Liver transplant (LT) is a vital, life-saving procedure for these patients. Demographic factors, including race, ethnicity, insurance status, and disease severity, influence LT rates and patient prognosis.
Methods: A retrospective chart review was conducted on adult patients with decompensated cirrhosis, admitted to our academic tertiary referral center located on the U.S./Mexico border, who met the criteria for a liver transplant between 2020 and 2024. Patients under the age of 18 and those with incomplete chart information were excluded. We evaluated both patients who received referrals for liver transplants and those who did not, analyzing demographic factors such as gender, insurance status, Area Deprivation Index (ADI), and comorbidities.
Results: Our study included 152 cirrhotic patients, of which 51 had a decompensating event as the primary reason for admission. The majority were male (52.9%) and Hispanic (80.4%), with an ADI of 8.72 ± 1.94 (Table 1). Insurance coverage varied: 35.2% were uninsured, 31.5% had Medicare, 25.9% had Medicaid, and 7.4% had private insurance coverage. Only 5 patients met criteria for liver transplant referral. Major reasons for non-referral included, lack of insurance (41.3%), ongoing alcohol or substance abuse (27.1%), severe cardiac or pulmonary disease (28.1%), and uncontrolled sepsis (18.8%). Of the 5 patients referred / transferred for LT, 3 underwent liver transplantation, 1 was rejected due to being a Jehovah's Witness, and 1 was lost to follow-up. Sadly, 70.6% of patients died during their hospital stay or within 90 days of hospitalization.
Discussion: Decompensated cirrhosis is a major mortality risk for MICU patients. Ahmed et al. found that the 2020 United Network for Organ Sharing liver allocation policy increased hospital costs by 12% in low-income areas, including our US/Mexico border hospital. This policy, along with barriers to equitable liver transplant (LT) access, worsens challenges for critically ill patients. Uninsured patients and ethnic minorities often present with advanced disease stages and lack LT access. Our study's low LT referral rate and high mortality highlight the urgent need for better care access, early intervention, and comprehensive management, especially for uninsured patients in an area with high ADI.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Shivangini Duggal, MD1, Bhavi Trivedi, MD2, Hedaia Algheriani, MD2, Michel Toutoungy, MD3, Li Guowei, MD4, Alejandro Robles, MD2, Sheldon Rao, MD2. P2930 - Evaluating Liver Transplant Referral Rates and Disparities Among Cirrhotic Patients: A Study in the Hispanic Population, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1TTUHSC, El Paso, TX; 2Texas Tech University Health Sciences Center, El Paso, TX; 3Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso, TX; 4Texas Tech University Health Sciences Center, EL Paso, TX
Introduction: End-stage liver disease significantly contributes to morbidity and mortality among ethnic minorities. Liver transplant (LT) is a vital, life-saving procedure for these patients. Demographic factors, including race, ethnicity, insurance status, and disease severity, influence LT rates and patient prognosis.
Methods: A retrospective chart review was conducted on adult patients with decompensated cirrhosis, admitted to our academic tertiary referral center located on the U.S./Mexico border, who met the criteria for a liver transplant between 2020 and 2024. Patients under the age of 18 and those with incomplete chart information were excluded. We evaluated both patients who received referrals for liver transplants and those who did not, analyzing demographic factors such as gender, insurance status, Area Deprivation Index (ADI), and comorbidities.
Results: Our study included 152 cirrhotic patients, of which 51 had a decompensating event as the primary reason for admission. The majority were male (52.9%) and Hispanic (80.4%), with an ADI of 8.72 ± 1.94 (Table 1). Insurance coverage varied: 35.2% were uninsured, 31.5% had Medicare, 25.9% had Medicaid, and 7.4% had private insurance coverage. Only 5 patients met criteria for liver transplant referral. Major reasons for non-referral included, lack of insurance (41.3%), ongoing alcohol or substance abuse (27.1%), severe cardiac or pulmonary disease (28.1%), and uncontrolled sepsis (18.8%). Of the 5 patients referred / transferred for LT, 3 underwent liver transplantation, 1 was rejected due to being a Jehovah's Witness, and 1 was lost to follow-up. Sadly, 70.6% of patients died during their hospital stay or within 90 days of hospitalization.
Discussion: Decompensated cirrhosis is a major mortality risk for MICU patients. Ahmed et al. found that the 2020 United Network for Organ Sharing liver allocation policy increased hospital costs by 12% in low-income areas, including our US/Mexico border hospital. This policy, along with barriers to equitable liver transplant (LT) access, worsens challenges for critically ill patients. Uninsured patients and ethnic minorities often present with advanced disease stages and lack LT access. Our study's low LT referral rate and high mortality highlight the urgent need for better care access, early intervention, and comprehensive management, especially for uninsured patients in an area with high ADI.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Shivangini Duggal indicated no relevant financial relationships.
Bhavi Trivedi indicated no relevant financial relationships.
Hedaia Algheriani indicated no relevant financial relationships.
Michel Toutoungy indicated no relevant financial relationships.
Li Guowei indicated no relevant financial relationships.
Alejandro Robles indicated no relevant financial relationships.
Sheldon Rao indicated no relevant financial relationships.
Shivangini Duggal, MD1, Bhavi Trivedi, MD2, Hedaia Algheriani, MD2, Michel Toutoungy, MD3, Li Guowei, MD4, Alejandro Robles, MD2, Sheldon Rao, MD2. P2930 - Evaluating Liver Transplant Referral Rates and Disparities Among Cirrhotic Patients: A Study in the Hispanic Population, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
