Monday Poster Session
Category: Liver
P2979 - Hepatocellular Carcinoma in Indian and Pakistani Immigrants in the United States: An Analysis of the SEER Database
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SB
Sheena Bhushan, MD
Northeast Georgia Medical Center
Buford, GA
Presenting Author(s)
Sheena Bhushan, MD1, Lisa S. Gambini, MPH2, Zainab Abbasi, MD3, Fnu Farukhuddin, MD4, Oluseyi Abidoye, MD5
1Northeast Georgia Medical Center, Buford, GA; 2Northeast Georgia Medical Center, Stonecrest, GA; 3Northeast Georgia Medical Center, Gainesville, GA; 4Warren Alpert Medical School of Brown University, Providence, RI; 5Mayo Clinic, Phoenix, AZ
Introduction: South Asian Americans (SAA), including Asian Indians and Pakistanis (I/P) are one of the fastest growing ethnic groups in the United States (US). Yet, there is minimal research on the prevalence of Hepatocellular Carcinoma (HCC), its survival trends and treatment utilization in this subgroup. The aim of this study was to examine the prevalence, survival patterns and treatment utilization in HCC among the I/P population compared to Whites and African Americans (AA).
Methods: Using Data from 17 SEER Research Plus Cancer registries, we identifed patients diagnosed with HCC between 2000-2021. We compared demographics, prevalence, survival, treatment utilization among SAA I/P, Whites and AA. Data were analyzed using frequencies, Kaplan Meir survival analysis, Cox proportional hazards regression and a logistic regression model.
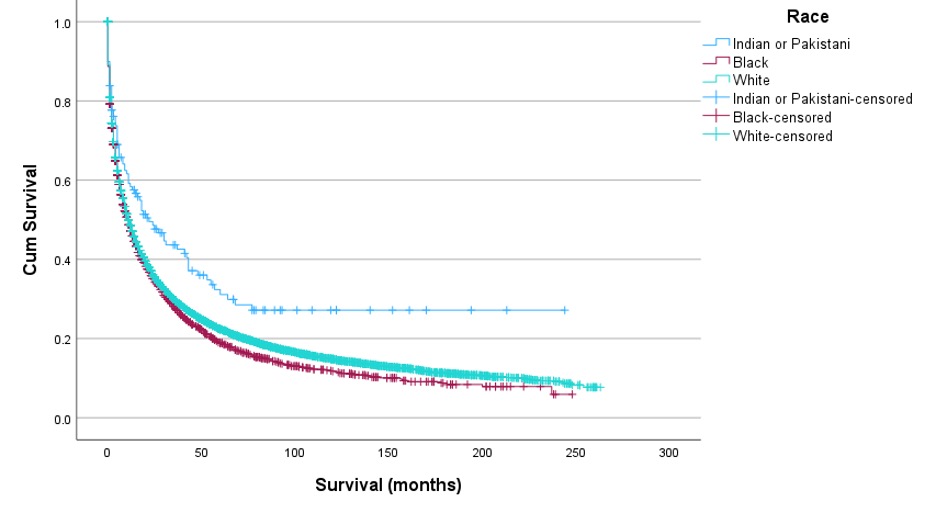
Results: Of the 16,592 patients, 0.8% (n=139) were I/P, 13.4% (n=2230) were AA and 85.7% (n=14223) were White. Survival in months was highest for I/P individuals (M=32.35, SD=46,29), followed by Whites (M=28.66, SD=44.13), and AA (M=25.22, SD=37.97) which was statistically significant {F(2, 16573)= 6.693, p=0.001}. The time from diagnosis to treatment in days was highest for AA (M=59.00, SD=62.21), followed by Whites (M=55.96, SD=59.11) and I/P (M=50.09, SD=51.34), but these differences were not statistically significant (p=0.135). The survival curves indicated that I/P had the longest estimated mean survival time (M=79.72 months), followed by Whites (M=49.50 months) and AA (M=41.79 months) (Image 1). The impact of race on survival time was assessed using a Cox proportional hazards regression analysis, which revealed that compared to Whites, I/P had a 47.7% higher risk of mortality (HR=1.477, p< 0.001), and Black individuals had a 37.7% higher risk of mortality (HR=1.377, p=0.003) (Table 2). A logistic regression analysis revealed that older individuals were less likely to undergo surgery (OR=0.987, 95% CI [0.983, 0.990], p < 0.001). Patients living in remote rural areas had lower odds of undergoing surgeries as compared to those in large metros (OR=0.694, 95% CI [0.535, 0.901], p= 0.006). Race was not a significant predictor of surgery likelihood. The model was statistically significant, χ²(14, N = 16,576) = 2,561.873, p < .001.
Discussion: Our findings highlight the disparities among minority immigrant groups in the United States. Culturally attuned public health initiatives and sampling is required to fully address these disparities.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sheena Bhushan, MD1, Lisa S. Gambini, MPH2, Zainab Abbasi, MD3, Fnu Farukhuddin, MD4, Oluseyi Abidoye, MD5. P2979 - Hepatocellular Carcinoma in Indian and Pakistani Immigrants in the United States: An Analysis of the SEER Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Northeast Georgia Medical Center, Buford, GA; 2Northeast Georgia Medical Center, Stonecrest, GA; 3Northeast Georgia Medical Center, Gainesville, GA; 4Warren Alpert Medical School of Brown University, Providence, RI; 5Mayo Clinic, Phoenix, AZ
Introduction: South Asian Americans (SAA), including Asian Indians and Pakistanis (I/P) are one of the fastest growing ethnic groups in the United States (US). Yet, there is minimal research on the prevalence of Hepatocellular Carcinoma (HCC), its survival trends and treatment utilization in this subgroup. The aim of this study was to examine the prevalence, survival patterns and treatment utilization in HCC among the I/P population compared to Whites and African Americans (AA).
Methods: Using Data from 17 SEER Research Plus Cancer registries, we identifed patients diagnosed with HCC between 2000-2021. We compared demographics, prevalence, survival, treatment utilization among SAA I/P, Whites and AA. Data were analyzed using frequencies, Kaplan Meir survival analysis, Cox proportional hazards regression and a logistic regression model.
Results: Of the 16,592 patients, 0.8% (n=139) were I/P, 13.4% (n=2230) were AA and 85.7% (n=14223) were White. Survival in months was highest for I/P individuals (M=32.35, SD=46,29), followed by Whites (M=28.66, SD=44.13), and AA (M=25.22, SD=37.97) which was statistically significant {F(2, 16573)= 6.693, p=0.001}. The time from diagnosis to treatment in days was highest for AA (M=59.00, SD=62.21), followed by Whites (M=55.96, SD=59.11) and I/P (M=50.09, SD=51.34), but these differences were not statistically significant (p=0.135). The survival curves indicated that I/P had the longest estimated mean survival time (M=79.72 months), followed by Whites (M=49.50 months) and AA (M=41.79 months) (Image 1). The impact of race on survival time was assessed using a Cox proportional hazards regression analysis, which revealed that compared to Whites, I/P had a 47.7% higher risk of mortality (HR=1.477, p< 0.001), and Black individuals had a 37.7% higher risk of mortality (HR=1.377, p=0.003) (Table 2). A logistic regression analysis revealed that older individuals were less likely to undergo surgery (OR=0.987, 95% CI [0.983, 0.990], p < 0.001). Patients living in remote rural areas had lower odds of undergoing surgeries as compared to those in large metros (OR=0.694, 95% CI [0.535, 0.901], p= 0.006). Race was not a significant predictor of surgery likelihood. The model was statistically significant, χ²(14, N = 16,576) = 2,561.873, p < .001.
Discussion: Our findings highlight the disparities among minority immigrant groups in the United States. Culturally attuned public health initiatives and sampling is required to fully address these disparities.
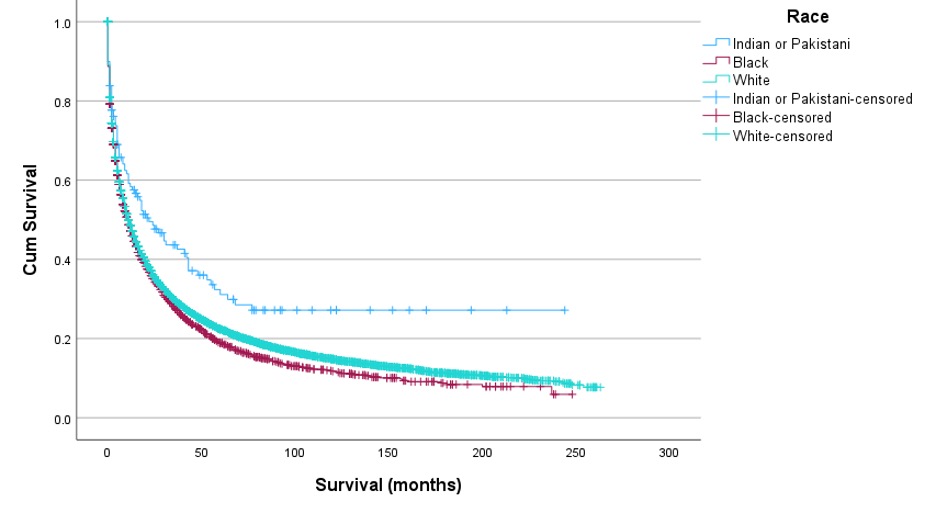
Figure: IMage 1: Survival by Race
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Sheena Bhushan indicated no relevant financial relationships.
Lisa Gambini indicated no relevant financial relationships.
Zainab Abbasi indicated no relevant financial relationships.
Fnu Farukhuddin indicated no relevant financial relationships.
Oluseyi Abidoye indicated no relevant financial relationships.
Sheena Bhushan, MD1, Lisa S. Gambini, MPH2, Zainab Abbasi, MD3, Fnu Farukhuddin, MD4, Oluseyi Abidoye, MD5. P2979 - Hepatocellular Carcinoma in Indian and Pakistani Immigrants in the United States: An Analysis of the SEER Database, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
