Monday Poster Session
Category: Liver
P2998 - A Case of Chronic Hepatitis E in a Liver Transplant Recipient
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- NV
Nevin Varghese, MD
Thomas Jefferson University Hospital
Philadelphia, PA
Presenting Author(s)
Nevin Varghese, MD1, Tammy Tran, MD, MBA1, Rachel Redfield, MD1, David A. Sass, MD, FACG2, Danielle M. Tholey, MD1
1Thomas Jefferson University Hospital, Philadelphia, PA; 2Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA
Introduction: Hepatitis E virus (HEV) causes 20 million new infections worldwide annually. Individuals with pre-existing liver disease, solid organ transplants (SOT), or immunosuppression are at risk for developing chronic HEV infection, which can rapidly progress to cirrhosis. Diagnosis can be challenging due to atypical presentation and lack of routine testing. We depict a case of a liver transplant (LT) recipient diagnosed with chronic HEV infection.
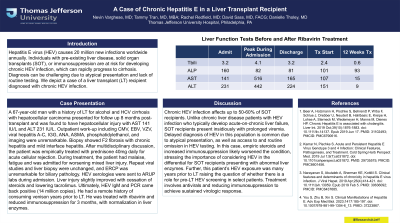
Case Description/Methods: A 67-year-old man with a history of LT for alcohol and HCV cirrhosis with hepatocellular carcinoma presented for follow up 8 months post-transplant and was found to have hepatocellular injury with AST 141 IU/L and ALT 231 IU/L. Outpatient work-up including CMV, EBV, VZV, viral hepatitis A-C, IGG, ANA, ASMA, phosphatidylethanol, and imaging were unremarkable. Biopsy showed F2 fibrosis with chronic hepatitis and mild interface hepatitis. After multidisciplinary discussion, the patient was empirically treated with prednisone 40 mg daily for acute cellular rejection. During treatment, the patient had malaise, fatigue and was admitted for worsening mixed liver injury. Repeat viral studies and liver biopsy were unchanged, and ERCP was unremarkable for biliary pathology. HEV serologies were sent to ARUP labs during admission. Liver injury slightly improved with cessation of steroids and lowering tacrolimus. Ultimately, HEV IgM and PCR came back positive (14 million copies). He had a remote history of consuming venison years prior to LT. He was treated with ribavirin and reduced immunosuppression for 3 months, with normalization in liver enzymes (Table 1).
Discussion: Chronic HEV infection affects up to 50-60% of SOT recipients. Unlike chronic liver disease patients with HEV infection who typically develop acute-on-chronic liver failure, SOT recipients present insidiously with prolonged viremia. Delayed diagnosis of HEV in this population is common due to atypical presentation, as well as access to and routine omission in HEV testing. In this case, empiric steroids and increased immunosuppression likely worsened the condition, stressing the importance of considering HEV in the differential for SOT recipients presenting with abnormal liver enzymes. Further, this patient’s HEV exposure was many years prior to LT raising the question of whether there is a role for pre-LT HEV screening in select patients. Treatment involves antivirals and reducing immunosuppression to achieve sustained virologic response.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Nevin Varghese, MD1, Tammy Tran, MD, MBA1, Rachel Redfield, MD1, David A. Sass, MD, FACG2, Danielle M. Tholey, MD1. P2998 - A Case of Chronic Hepatitis E in a Liver Transplant Recipient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Thomas Jefferson University Hospital, Philadelphia, PA; 2Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA
Introduction: Hepatitis E virus (HEV) causes 20 million new infections worldwide annually. Individuals with pre-existing liver disease, solid organ transplants (SOT), or immunosuppression are at risk for developing chronic HEV infection, which can rapidly progress to cirrhosis. Diagnosis can be challenging due to atypical presentation and lack of routine testing. We depict a case of a liver transplant (LT) recipient diagnosed with chronic HEV infection.
Case Description/Methods: A 67-year-old man with a history of LT for alcohol and HCV cirrhosis with hepatocellular carcinoma presented for follow up 8 months post-transplant and was found to have hepatocellular injury with AST 141 IU/L and ALT 231 IU/L. Outpatient work-up including CMV, EBV, VZV, viral hepatitis A-C, IGG, ANA, ASMA, phosphatidylethanol, and imaging were unremarkable. Biopsy showed F2 fibrosis with chronic hepatitis and mild interface hepatitis. After multidisciplinary discussion, the patient was empirically treated with prednisone 40 mg daily for acute cellular rejection. During treatment, the patient had malaise, fatigue and was admitted for worsening mixed liver injury. Repeat viral studies and liver biopsy were unchanged, and ERCP was unremarkable for biliary pathology. HEV serologies were sent to ARUP labs during admission. Liver injury slightly improved with cessation of steroids and lowering tacrolimus. Ultimately, HEV IgM and PCR came back positive (14 million copies). He had a remote history of consuming venison years prior to LT. He was treated with ribavirin and reduced immunosuppression for 3 months, with normalization in liver enzymes (Table 1).
Discussion: Chronic HEV infection affects up to 50-60% of SOT recipients. Unlike chronic liver disease patients with HEV infection who typically develop acute-on-chronic liver failure, SOT recipients present insidiously with prolonged viremia. Delayed diagnosis of HEV in this population is common due to atypical presentation, as well as access to and routine omission in HEV testing. In this case, empiric steroids and increased immunosuppression likely worsened the condition, stressing the importance of considering HEV in the differential for SOT recipients presenting with abnormal liver enzymes. Further, this patient’s HEV exposure was many years prior to LT raising the question of whether there is a role for pre-LT HEV screening in select patients. Treatment involves antivirals and reducing immunosuppression to achieve sustained virologic response.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Nevin Varghese indicated no relevant financial relationships.
Tammy Tran indicated no relevant financial relationships.
Rachel Redfield indicated no relevant financial relationships.
David Sass indicated no relevant financial relationships.
Danielle Tholey: Merck – see above – editor for merck manual educational resource.
Nevin Varghese, MD1, Tammy Tran, MD, MBA1, Rachel Redfield, MD1, David A. Sass, MD, FACG2, Danielle M. Tholey, MD1. P2998 - A Case of Chronic Hepatitis E in a Liver Transplant Recipient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
