Monday Poster Session
Category: Liver
P3003 - Low-Phospholipid Associated Cholelithiasis Syndrome – An Uncommon Cause of Hepatectomy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Brenton Davis, MD
Kaiser Permanente
San Francisco, CA
Presenting Author(s)
Brenton Davis, MD, Max Goldman, MD, Nizar Mukhtar, MD
Kaiser Permanente, San Francisco, CA
Introduction: Low-phospholipid associated cholelithiasis (LPAC) syndrome is caused by a range of genetic mutations in proteins related to bile transport like ABCB4, which creates a more inflammatory and lithogenic bile. Initially thought to be uncommon, some studies show LPAC constitutes 0.5-1.9% of adults with symptomatic cholelithiasis. Disease severity is variable based on the type and number of inherited genetic mutations. ABCB4 biallelic mutation has been shown to cause early onset of severe symptoms with increased risk of cholangitis and hepatobiliary cancer. Treatment with ursodeoxycholic acid (UDCA) has been shown to be effective. With more cases being noted, different inciting genotypes are being documented. This case illustrates the importance of early diagnosis and treatment of LPAC to avoid multiple procedures and complications requiring surgical intervention.
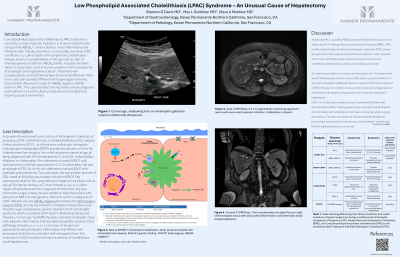
Case Description/Methods: A 50-year-old woman with prior history of cholelithiasis (CL), pruritis during pregnancy, choledocholithiasis (CDL) despite cholecystectomy (CCY) and three prior endoscopic retrograde cholangiopancreatography (ERCP) procedures was seen in clinic for indeterminate liver imaging. Her initial symptoms started at age 36 with pruritis during pregnancy which was complicated by CL and CDL without biliary dilatation or cholecystitis. She underwent successful ERCP with sphincterotomy and had a post-partum CCY. Six years after, she had another episode of CDL for which she underwent a second ERCP with extended sphincterotomy. Two years later, she had another episode of CDL noted on EUS that was treated with a third ERCP. She experienced relief for two years before re-experiencing biliary colic at age 48. During her workup, a CT scan showed a 2.9 x 3.1 x 3.8cm region of hypoenhancement in segment 6 of the liver. She was referred to surgery where she was started on high dose UDCA with plans for an MRI liver and genetics referral to confirm a diagnosis of LPAC. Notably she was ABCB4 negative but positive for heterozygous variant DHCR7, an enzyme involved in cholesterol biosynthesis. MRI showed a retained intrahepatic stone with adjacent inflammation that was laparoscopically resected.
Discussion: LPAC is an increasingly recognized cause of symptomatic lithiasis that responds well to UDCA. Identifying and treating patients early in their disease course may help avoid complex intrahepatic stone formation and complications that require endoscopic or surgical interventions.
Disclosures:
Brenton Davis, MD, Max Goldman, MD, Nizar Mukhtar, MD. P3003 - Low-Phospholipid Associated Cholelithiasis Syndrome – An Uncommon Cause of Hepatectomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Kaiser Permanente, San Francisco, CA
Introduction: Low-phospholipid associated cholelithiasis (LPAC) syndrome is caused by a range of genetic mutations in proteins related to bile transport like ABCB4, which creates a more inflammatory and lithogenic bile. Initially thought to be uncommon, some studies show LPAC constitutes 0.5-1.9% of adults with symptomatic cholelithiasis. Disease severity is variable based on the type and number of inherited genetic mutations. ABCB4 biallelic mutation has been shown to cause early onset of severe symptoms with increased risk of cholangitis and hepatobiliary cancer. Treatment with ursodeoxycholic acid (UDCA) has been shown to be effective. With more cases being noted, different inciting genotypes are being documented. This case illustrates the importance of early diagnosis and treatment of LPAC to avoid multiple procedures and complications requiring surgical intervention.
Case Description/Methods: A 50-year-old woman with prior history of cholelithiasis (CL), pruritis during pregnancy, choledocholithiasis (CDL) despite cholecystectomy (CCY) and three prior endoscopic retrograde cholangiopancreatography (ERCP) procedures was seen in clinic for indeterminate liver imaging. Her initial symptoms started at age 36 with pruritis during pregnancy which was complicated by CL and CDL without biliary dilatation or cholecystitis. She underwent successful ERCP with sphincterotomy and had a post-partum CCY. Six years after, she had another episode of CDL for which she underwent a second ERCP with extended sphincterotomy. Two years later, she had another episode of CDL noted on EUS that was treated with a third ERCP. She experienced relief for two years before re-experiencing biliary colic at age 48. During her workup, a CT scan showed a 2.9 x 3.1 x 3.8cm region of hypoenhancement in segment 6 of the liver. She was referred to surgery where she was started on high dose UDCA with plans for an MRI liver and genetics referral to confirm a diagnosis of LPAC. Notably she was ABCB4 negative but positive for heterozygous variant DHCR7, an enzyme involved in cholesterol biosynthesis. MRI showed a retained intrahepatic stone with adjacent inflammation that was laparoscopically resected.
Discussion: LPAC is an increasingly recognized cause of symptomatic lithiasis that responds well to UDCA. Identifying and treating patients early in their disease course may help avoid complex intrahepatic stone formation and complications that require endoscopic or surgical interventions.
Disclosures:
Brenton Davis indicated no relevant financial relationships.
Max Goldman indicated no relevant financial relationships.
Nizar Mukhtar indicated no relevant financial relationships.
Brenton Davis, MD, Max Goldman, MD, Nizar Mukhtar, MD. P3003 - Low-Phospholipid Associated Cholelithiasis Syndrome – An Uncommon Cause of Hepatectomy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
