Monday Poster Session
Category: Liver
P3012 - Steatotic Liver Disease Arising in an Asymptomatic 20-Year-Old Male With Growth Hormone Deficiency
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Nicole Wiebe, BSc, BA, MD
Dalhousie University
Halifax, NS, Canada
Presenting Author(s)
Nicole Wiebe, BSc, BA, MD, Ashley Stueck, MD, Magnus McLeod, MD
Dalhousie University, Halifax, NS, Canada
Introduction: Steatotic liver disease (SLD) may be caused by the presence of cardiometabolic risk factors, viral hepatitis, genetic diseases, malnutrition, or panhypopituitarism. SLD can advance to steatohepatitis where lipid accumulation is accompanied by inflammation and hepatocellular damage. SLD is associated with pituitary dysfunction, especially growth hormone deficiency, as insulin resistance leads to lipid build-up in hepatocytes and oxidative stress. Growth hormone replacement therapy may improve liver steatosis and fibrosis in patients with hypopituitarism.
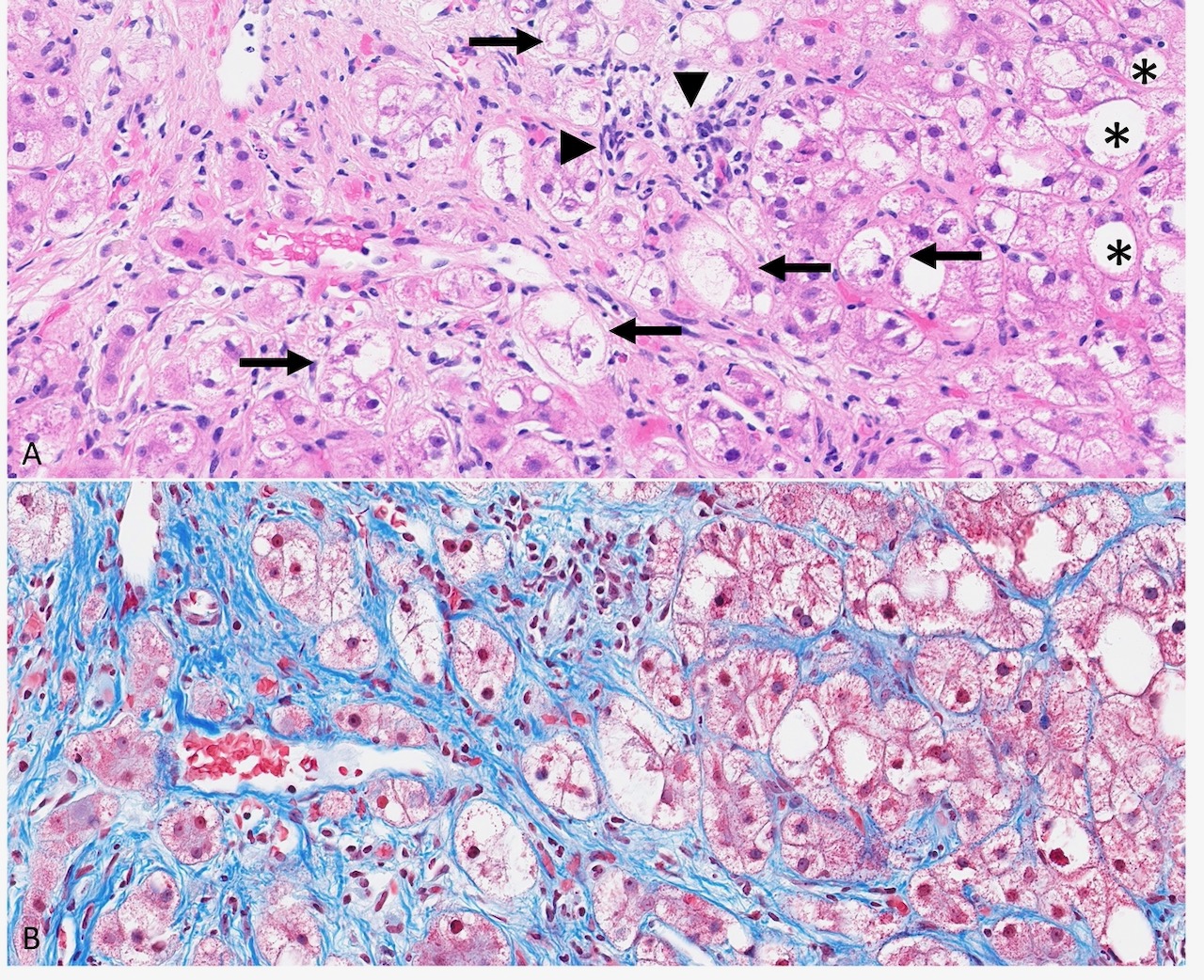
Case Description/Methods: We report a case of a 20-year-old male referred to Hepatology with abnormal liver enzymes. His medical history included panhypopituitarism from a surgically resected pituitary mass, for which he was treated with levothyroxine, hydrocortisone, growth hormone, and testosterone. He presented to Hepatology with markedly elevated liver enzymes (alanine transaminase 556 U/L, aspartate transaminase 258 U/L, alkaline phosphatase 175 U/L, gamma-glutamyl transferase 363 U/L), normal liver function (total bilirubin 15.9 mmol/L, international normalized ratio 1.0, albumin 50 g/L), obesity (weight 93 kg), dyslipidemia (cholesterol 7.2 mmol/L, low-density lipoprotein 4.8 mmol/L), and no evidence of extrahepatic manifestations of chronic liver disease. Work-up for secondary causes of liver disease including infectious, autoimmune, drug-induced, and genetic were negative. Abdominal ultrasound revealed moderate hepatic steatosis with mild hepatomegaly and splenomegaly. His liver enzymes remained elevated and his biochemical liver function remained normal despite discontinuation of hepatotoxic medications. Liver biopsy showed grade II/III steatohepatitis with stage III-IV fibrosis (Figure 1) and FibroScan liver stiffness score was 21.8 kPa. The biopsy results suggested that panhypopituitarism, specifically growth hormone deficiency, and metabolic dysfunction, contributed to his liver disease.
Discussion: This is a unique case of an aggressive form of SLD that likely developed after the onset of altered growth hormone signaling and growth hormone replacement therapy did not improve abnormal liver enzymes or liver damage. Physicians should recognize SLD as a complication of growth hormone deficiency and follow patients with bloodwork and imaging given the risk of disease progression.
Disclosures:
Nicole Wiebe, BSc, BA, MD, Ashley Stueck, MD, Magnus McLeod, MD. P3012 - Steatotic Liver Disease Arising in an Asymptomatic 20-Year-Old Male With Growth Hormone Deficiency, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Dalhousie University, Halifax, NS, Canada
Introduction: Steatotic liver disease (SLD) may be caused by the presence of cardiometabolic risk factors, viral hepatitis, genetic diseases, malnutrition, or panhypopituitarism. SLD can advance to steatohepatitis where lipid accumulation is accompanied by inflammation and hepatocellular damage. SLD is associated with pituitary dysfunction, especially growth hormone deficiency, as insulin resistance leads to lipid build-up in hepatocytes and oxidative stress. Growth hormone replacement therapy may improve liver steatosis and fibrosis in patients with hypopituitarism.
Case Description/Methods: We report a case of a 20-year-old male referred to Hepatology with abnormal liver enzymes. His medical history included panhypopituitarism from a surgically resected pituitary mass, for which he was treated with levothyroxine, hydrocortisone, growth hormone, and testosterone. He presented to Hepatology with markedly elevated liver enzymes (alanine transaminase 556 U/L, aspartate transaminase 258 U/L, alkaline phosphatase 175 U/L, gamma-glutamyl transferase 363 U/L), normal liver function (total bilirubin 15.9 mmol/L, international normalized ratio 1.0, albumin 50 g/L), obesity (weight 93 kg), dyslipidemia (cholesterol 7.2 mmol/L, low-density lipoprotein 4.8 mmol/L), and no evidence of extrahepatic manifestations of chronic liver disease. Work-up for secondary causes of liver disease including infectious, autoimmune, drug-induced, and genetic were negative. Abdominal ultrasound revealed moderate hepatic steatosis with mild hepatomegaly and splenomegaly. His liver enzymes remained elevated and his biochemical liver function remained normal despite discontinuation of hepatotoxic medications. Liver biopsy showed grade II/III steatohepatitis with stage III-IV fibrosis (Figure 1) and FibroScan liver stiffness score was 21.8 kPa. The biopsy results suggested that panhypopituitarism, specifically growth hormone deficiency, and metabolic dysfunction, contributed to his liver disease.
Discussion: This is a unique case of an aggressive form of SLD that likely developed after the onset of altered growth hormone signaling and growth hormone replacement therapy did not improve abnormal liver enzymes or liver damage. Physicians should recognize SLD as a complication of growth hormone deficiency and follow patients with bloodwork and imaging given the risk of disease progression.
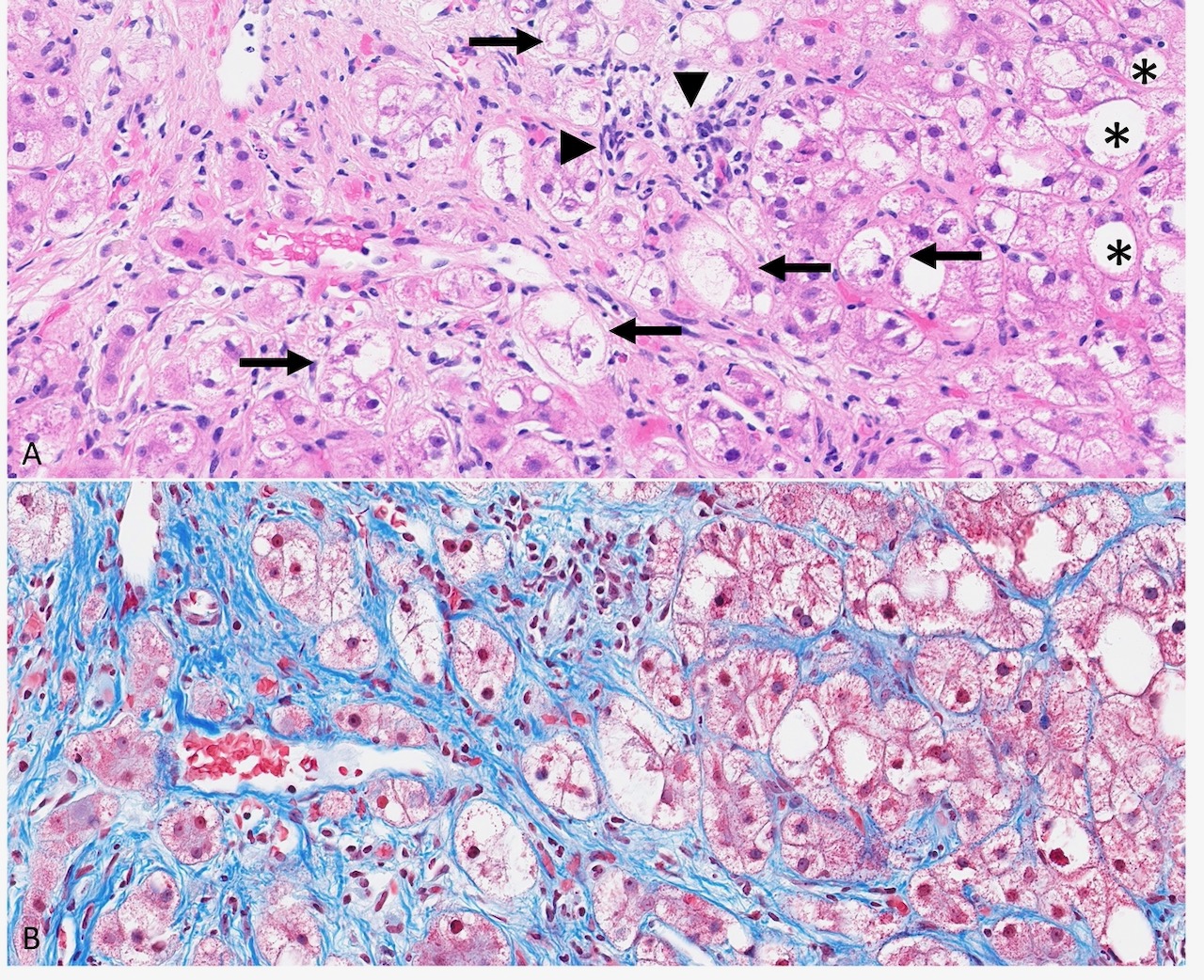
Figure: A. Liver parenchyma showing macrovesicular steatosis (*) and steatohepatitis including hepatocytes with ballooning degeneration and poorly-formed Mallory-Denk bodies (arrows) and inflammation (arrowheads). B. The same area with extensive pericellular “chicken wire” fibrosis. Masson trichrome stain, 300x.
Disclosures:
Nicole Wiebe indicated no relevant financial relationships.
Ashley Stueck indicated no relevant financial relationships.
Magnus McLeod indicated no relevant financial relationships.
Nicole Wiebe, BSc, BA, MD, Ashley Stueck, MD, Magnus McLeod, MD. P3012 - Steatotic Liver Disease Arising in an Asymptomatic 20-Year-Old Male With Growth Hormone Deficiency, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
