Monday Poster Session
Category: Liver
P3013 - Difficult Diagnosis of Disseminated Cryptococcosis in a Patient With Cirrhosis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Emma Russell, BS
Texas A&M School of Medicine
Round Rock, TX
Presenting Author(s)
Emma Russell, BS1, Yizhong Wu, MD2, Manuel Garza, MD, MS3, Sanjay Prasad, MD3, Kim Minh Le, DO4, Wasay A. Mohajir, DO3, MaryAnn Tran, MD3, Raja K. Dhanekula, MS, MD, MBBS5
1Texas A&M School of Medicine, Round Rock, TX; 2Baylor Scott & White Medical Center, Georgetown, TX; 3Baylor Scott & White Medical Center, Round Rock, TX; 4Baylor Scott & White Medical Center, Austin, TX; 5Baylor Scott and White Round Rock, Round Rock, TX
Introduction: Patients with cirrhosis are at higher risk for spontaneous bacterial peritonitis (SBP), urinary tract infections (UTI), and infection by opportunistic organisms. Cirrhosis is an independent risk factor for cryptococcal infection, a disease where meningeal involvement is associated with high morbidity and mortality. We present a case of new onset seizures and cerebral infarcts in a patient with cirrhosis eventually diagnosed as cryptococcal meningitis.
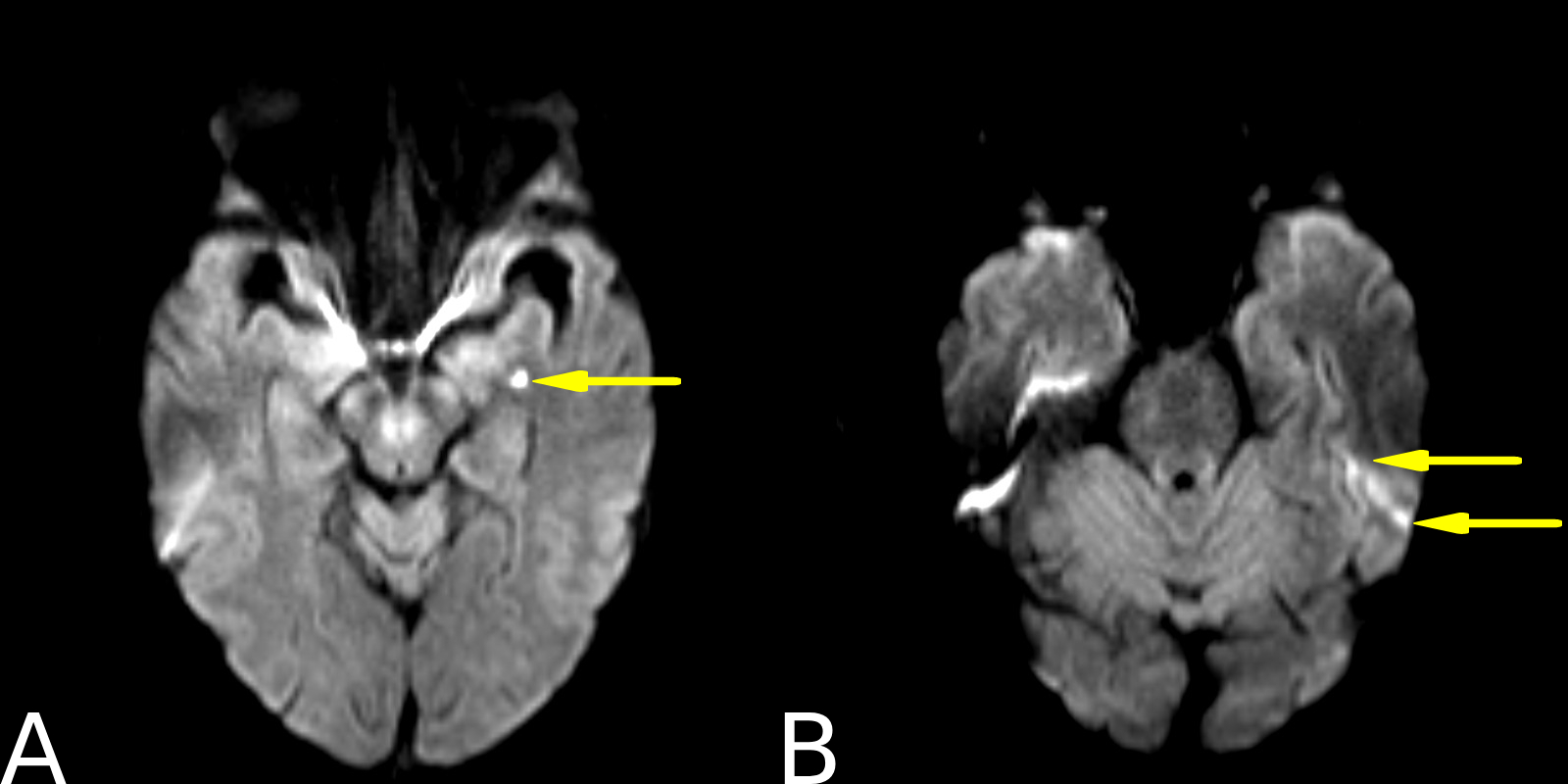
Case Description/Methods: A 66-year-old man with decompensated alcohol related cirrhosis (MELD 3.0 score 28, Child-Pugh class C) and HCC presented for new body stiffness and shaking in the setting of one week of headaches. Vital signs were unremarkable. The physical exam was pertinent for a distended but non-tender abdomen, with no focal deficits. He last used alcohol two months prior. MRI showed acute/subacute basal ganglia and temporal infarcts (Figure 1). His seizures resolved after starting levetiracetam and was discharged. One week later, he returned to the hospital with intermittent fevers and ascitic fluid cultures that grew gram negative rods. On the physical exam, he was alert and oriented with a distended, tender abdomen. He was treated for SBP. Within five days, his mentation progressively declined, and he developed asterixis. Lactulose was up titrated and rifaximin was added. His ammonia level was 21 mcg/dL. Despite treatment, he became minimally arousable. He did not exhibit evidence of UTI or pneumonia, and there were no signs of blood loss. Further work-up revealed an elevated cryptococcus antigen of 1:4096 in serum. Subsequent lumbar puncture revealed an opening pressure of 29 cm H2O, protein 357.2 mg/dL, glucose 2 mg/100mL, and positive cryptococcus PCR in cerebrospinal fluid (CSF). Amphotericin B and flucytosine were initiated, and the patient was transferred for higher level of care and serial lumbar punctures. Unfortunately, the patient expired shortly after.
Discussion: This unique case highlights the importance of investigating other etiologies when a cirrhotic patient declines despite appropriate medical therapy. Alternative diagnoses such as opportunistic infections are high on the differential in patients with decompensated cirrhosis given their immunocompromised state. Systemic diagnostic reasoning is paramount for the diagnosis of disseminated cryptococcosis, given it is an easily missed, aggressive, and life-threatening disease.
Disclosures:
Emma Russell, BS1, Yizhong Wu, MD2, Manuel Garza, MD, MS3, Sanjay Prasad, MD3, Kim Minh Le, DO4, Wasay A. Mohajir, DO3, MaryAnn Tran, MD3, Raja K. Dhanekula, MS, MD, MBBS5. P3013 - Difficult Diagnosis of Disseminated Cryptococcosis in a Patient With Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Texas A&M School of Medicine, Round Rock, TX; 2Baylor Scott & White Medical Center, Georgetown, TX; 3Baylor Scott & White Medical Center, Round Rock, TX; 4Baylor Scott & White Medical Center, Austin, TX; 5Baylor Scott and White Round Rock, Round Rock, TX
Introduction: Patients with cirrhosis are at higher risk for spontaneous bacterial peritonitis (SBP), urinary tract infections (UTI), and infection by opportunistic organisms. Cirrhosis is an independent risk factor for cryptococcal infection, a disease where meningeal involvement is associated with high morbidity and mortality. We present a case of new onset seizures and cerebral infarcts in a patient with cirrhosis eventually diagnosed as cryptococcal meningitis.
Case Description/Methods: A 66-year-old man with decompensated alcohol related cirrhosis (MELD 3.0 score 28, Child-Pugh class C) and HCC presented for new body stiffness and shaking in the setting of one week of headaches. Vital signs were unremarkable. The physical exam was pertinent for a distended but non-tender abdomen, with no focal deficits. He last used alcohol two months prior. MRI showed acute/subacute basal ganglia and temporal infarcts (Figure 1). His seizures resolved after starting levetiracetam and was discharged. One week later, he returned to the hospital with intermittent fevers and ascitic fluid cultures that grew gram negative rods. On the physical exam, he was alert and oriented with a distended, tender abdomen. He was treated for SBP. Within five days, his mentation progressively declined, and he developed asterixis. Lactulose was up titrated and rifaximin was added. His ammonia level was 21 mcg/dL. Despite treatment, he became minimally arousable. He did not exhibit evidence of UTI or pneumonia, and there were no signs of blood loss. Further work-up revealed an elevated cryptococcus antigen of 1:4096 in serum. Subsequent lumbar puncture revealed an opening pressure of 29 cm H2O, protein 357.2 mg/dL, glucose 2 mg/100mL, and positive cryptococcus PCR in cerebrospinal fluid (CSF). Amphotericin B and flucytosine were initiated, and the patient was transferred for higher level of care and serial lumbar punctures. Unfortunately, the patient expired shortly after.
Discussion: This unique case highlights the importance of investigating other etiologies when a cirrhotic patient declines despite appropriate medical therapy. Alternative diagnoses such as opportunistic infections are high on the differential in patients with decompensated cirrhosis given their immunocompromised state. Systemic diagnostic reasoning is paramount for the diagnosis of disseminated cryptococcosis, given it is an easily missed, aggressive, and life-threatening disease.
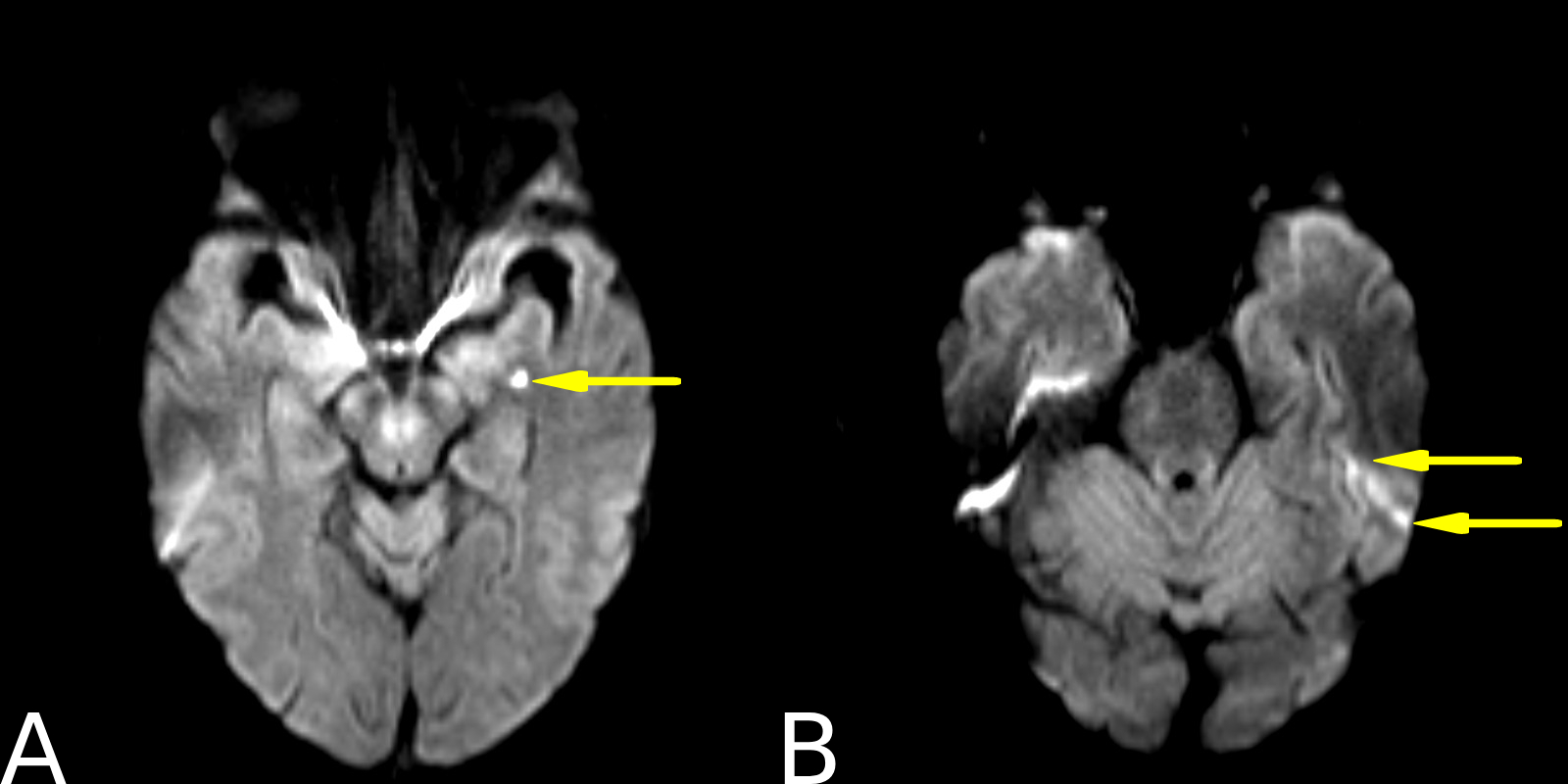
Figure: Figure 1. A: Basal ganglia punctate infarct found on MRI during initial ED visit. B: Temporal lobe infarcts found on the same MRI.
Disclosures:
Emma Russell indicated no relevant financial relationships.
Yizhong Wu indicated no relevant financial relationships.
Manuel Garza indicated no relevant financial relationships.
Sanjay Prasad indicated no relevant financial relationships.
Kim Minh Le indicated no relevant financial relationships.
Wasay Mohajir indicated no relevant financial relationships.
MaryAnn Tran indicated no relevant financial relationships.
Raja Dhanekula indicated no relevant financial relationships.
Emma Russell, BS1, Yizhong Wu, MD2, Manuel Garza, MD, MS3, Sanjay Prasad, MD3, Kim Minh Le, DO4, Wasay A. Mohajir, DO3, MaryAnn Tran, MD3, Raja K. Dhanekula, MS, MD, MBBS5. P3013 - Difficult Diagnosis of Disseminated Cryptococcosis in a Patient With Cirrhosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
