Monday Poster Session
Category: Liver
P3076 - Drug-Induced Autoimmune-Like Hepatitis and Stevens Johnsons Syndrome Secondary to Levetiracetam
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Dalton M. Caviness, MD
University of Alabama at Birmingham
Gardendale, AL
Presenting Author(s)
Dalton M. Caviness, MD1, Kristin Olson, MD, PhD, MPH2, Meagan Gray, MD3
1University of Alabama at Birmingham, Gardendale, AL; 2University of Alabama at Birmingham, Birmingham, AL; 3The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
Introduction: Drug-induced liver injury (DILI) is common and can mimic both acute and chronic liver disease. A subset of patients with DILI will have drug induced autoimmune-like hepatitis (DI-ALH), which can present at any time during the course of treatment. DI-ALH is well described with medications such as nitrofurantoin and infliximab, but herein we present a unique case of DI-ALH secondary to levetiracetam.
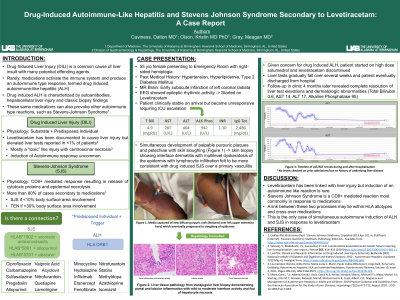
Case Description/Methods: A 55 year-old female presented to the Emergency Room with right sided hemiplegia. Her history was significant for hypertension, hyperlipidemia, and type 2 diabetes mellitus managed on appropriate therapy. Magnetic resonance imaging confirmed a new early subacute infarction of the left coronal radiata and she was started on aspirin and clopidogrel. Subsequently, she developed temporal intermittent rhythmic delta activity on electroencephalogram and was initiated on levetiracetam. Approximately three weeks later patient became unresponsive necessitating transfer to the intensive care unit and liver tests were found to be significantly elevated with total bilirubin 4.9 mg/dL, AST 287 U/L, ALT 404 U/L and alkaline phosphatase 942 U/L. Her INR was 1.10. Her liver tests had not been previously tested at our facility. Extensive serologic workup was significant only for a total immunoglobulin G of 2,486 mg/dL. A liver biopsy showed portal and lobular inflammation with mild to moderate interface activity and foci of hepatocyte necrosis (Figure 1). She simultaneously developed palpable purpuric plaques and petechiae felt to be consistent with Stevens Johnson Syndrome (SJS). Given concern for DI-ALH and DI-SJS intravenous solumedrol was started and her levetiracetam was discontinued. She gradually improved and was able to be discharged off of any steroids or immunosuppression. Follow-up in the clinic 6 months later revealed complete resolution of liver test elevations and dermatologic abnormalities (TB 0.6, AST 14, ALT 17, AP 95).
Discussion: Levetiracetam has been previously instigated in rare instances of liver enzyme elevations and Stevens Johnson Syndrome. Here, we present a unique case of DI-ALH secondary to levetiracetam which resolved with drug discontinuation. Early identification of DILI and DI-ALH is crucial not only for patient recovery but also to avoid use of unnecessary immunosuppression. There has been only one previous case published of DI-ALH secondary to levetiracetam and we hope that this second case will further serve to raise awareness of this relationship.
Disclosures:
Dalton M. Caviness, MD1, Kristin Olson, MD, PhD, MPH2, Meagan Gray, MD3. P3076 - Drug-Induced Autoimmune-Like Hepatitis and Stevens Johnsons Syndrome Secondary to Levetiracetam, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Alabama at Birmingham, Gardendale, AL; 2University of Alabama at Birmingham, Birmingham, AL; 3The University of Alabama at Birmingham Heersink School of Medicine, Birmingham, AL
Introduction: Drug-induced liver injury (DILI) is common and can mimic both acute and chronic liver disease. A subset of patients with DILI will have drug induced autoimmune-like hepatitis (DI-ALH), which can present at any time during the course of treatment. DI-ALH is well described with medications such as nitrofurantoin and infliximab, but herein we present a unique case of DI-ALH secondary to levetiracetam.
Case Description/Methods: A 55 year-old female presented to the Emergency Room with right sided hemiplegia. Her history was significant for hypertension, hyperlipidemia, and type 2 diabetes mellitus managed on appropriate therapy. Magnetic resonance imaging confirmed a new early subacute infarction of the left coronal radiata and she was started on aspirin and clopidogrel. Subsequently, she developed temporal intermittent rhythmic delta activity on electroencephalogram and was initiated on levetiracetam. Approximately three weeks later patient became unresponsive necessitating transfer to the intensive care unit and liver tests were found to be significantly elevated with total bilirubin 4.9 mg/dL, AST 287 U/L, ALT 404 U/L and alkaline phosphatase 942 U/L. Her INR was 1.10. Her liver tests had not been previously tested at our facility. Extensive serologic workup was significant only for a total immunoglobulin G of 2,486 mg/dL. A liver biopsy showed portal and lobular inflammation with mild to moderate interface activity and foci of hepatocyte necrosis (Figure 1). She simultaneously developed palpable purpuric plaques and petechiae felt to be consistent with Stevens Johnson Syndrome (SJS). Given concern for DI-ALH and DI-SJS intravenous solumedrol was started and her levetiracetam was discontinued. She gradually improved and was able to be discharged off of any steroids or immunosuppression. Follow-up in the clinic 6 months later revealed complete resolution of liver test elevations and dermatologic abnormalities (TB 0.6, AST 14, ALT 17, AP 95).
Discussion: Levetiracetam has been previously instigated in rare instances of liver enzyme elevations and Stevens Johnson Syndrome. Here, we present a unique case of DI-ALH secondary to levetiracetam which resolved with drug discontinuation. Early identification of DILI and DI-ALH is crucial not only for patient recovery but also to avoid use of unnecessary immunosuppression. There has been only one previous case published of DI-ALH secondary to levetiracetam and we hope that this second case will further serve to raise awareness of this relationship.
Disclosures:
Dalton Caviness indicated no relevant financial relationships.
Kristin Olson indicated no relevant financial relationships.
Meagan Gray: Novo Nordisk – Consultant.
Dalton M. Caviness, MD1, Kristin Olson, MD, PhD, MPH2, Meagan Gray, MD3. P3076 - Drug-Induced Autoimmune-Like Hepatitis and Stevens Johnsons Syndrome Secondary to Levetiracetam, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
