Monday Poster Session
Category: Liver
P3079 - Progressive Familial Intrahepatic Cholestasis: A Histological Conundrum
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Kishore Karri, MBBS, MD
University of Kentucky
Lexington, KY
Presenting Author(s)
Nimish Thakral, MD1, Kishore Karri, MBBS, MD1, Jerapas Thongpiya, MD2
1University of Kentucky, Lexington, KY; 2Texas Tech University Health Sciences Center, Lubbock, TX
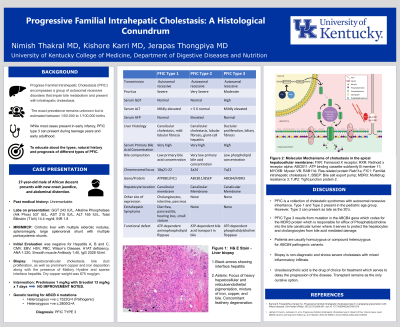
Introduction: Progress Familial Intrahepatic Cholestasis (PFIC) encompasses a group of autosomal recessive disorders that impair bile metabolism and present with intrahepatic cholestasis. The exact prevalence remains unknown but is estimated between 1/50,000 to 1/10,000 births. Genetic testing is diagnostic. Liver biopsy often shows cholestasis, bile duct proliferation, and portal fibrosis. Here we describe a case of PFIC type 3 presenting with hemosiderosis and Mallory hyaline, the association of which has not been described in literature before.
Case Description/Methods: A 26-year-old male of West African descent presented with 4 weeks of jaundice. Past history and family history were not available since the patient was adopted. Labs on admission were alkaline phosphatase 537I U/L, AST 215 U/L, ALT 65 U/L, T bili 13.2 mg/dl, and GGT 470 U/L. Initial testing for causes of liver disease was negative for Hepatitis A, B, and C, CMV, EBV, HSV, Autoimmune Hepatitis (AIH), Primary Biliary Cholangitis, and Ceruloplasmin levels were normal. MRCP showed cirrhosis, and stigmata of portal hypertension without any altered biliary anatomy. Liver biopsy showed prominent hepatocanalicular cholestasis, bile duct proliferation, as well as prominent copper and iron deposition along with presence of Mallory Hyaline and sparse interface hepatitis. Dry copper weight was 670 mcg/gm. Genetic testing was sent for Wilson’s Disease (ATP7B) and PFIC type 3 (ABCB4). The patient was subsequently found to be heterozygous positive for two different genetic mutations of ABCB4 (one pathologic, and another of undetermined significance), thereby confirming the diagnosis of PFIC Type 3. The patient underwent liver transplant with subsequent resolution of his liver disease.
Discussion: PFIC Type 3 is caused by a defect in the ABCB4 gene on chromosome 7 which transcribes the MDR3 protein. MDR3 is responsible for biliary excretion at the hepatocyte membrane. The clinical phenotype varies from neonatal cholestasis and cirrhosis in young adults. Diagnosis can be tricky and requires detailed serological evaluation with genetic analysis for confirmation. Most patients have homozygous pathological mutation of ABCB4. However, less than 10% of patients (including ours) have only pathological mutations. UDCA is the first line of treatment with transplant being curative. Clinicians must be aware of this condition as early treatment and transplantation can prevent unnecessary morbidity and reduce mortality.
Disclosures:
Nimish Thakral, MD1, Kishore Karri, MBBS, MD1, Jerapas Thongpiya, MD2. P3079 - Progressive Familial Intrahepatic Cholestasis: A Histological Conundrum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Kentucky, Lexington, KY; 2Texas Tech University Health Sciences Center, Lubbock, TX
Introduction: Progress Familial Intrahepatic Cholestasis (PFIC) encompasses a group of autosomal recessive disorders that impair bile metabolism and present with intrahepatic cholestasis. The exact prevalence remains unknown but is estimated between 1/50,000 to 1/10,000 births. Genetic testing is diagnostic. Liver biopsy often shows cholestasis, bile duct proliferation, and portal fibrosis. Here we describe a case of PFIC type 3 presenting with hemosiderosis and Mallory hyaline, the association of which has not been described in literature before.
Case Description/Methods: A 26-year-old male of West African descent presented with 4 weeks of jaundice. Past history and family history were not available since the patient was adopted. Labs on admission were alkaline phosphatase 537I U/L, AST 215 U/L, ALT 65 U/L, T bili 13.2 mg/dl, and GGT 470 U/L. Initial testing for causes of liver disease was negative for Hepatitis A, B, and C, CMV, EBV, HSV, Autoimmune Hepatitis (AIH), Primary Biliary Cholangitis, and Ceruloplasmin levels were normal. MRCP showed cirrhosis, and stigmata of portal hypertension without any altered biliary anatomy. Liver biopsy showed prominent hepatocanalicular cholestasis, bile duct proliferation, as well as prominent copper and iron deposition along with presence of Mallory Hyaline and sparse interface hepatitis. Dry copper weight was 670 mcg/gm. Genetic testing was sent for Wilson’s Disease (ATP7B) and PFIC type 3 (ABCB4). The patient was subsequently found to be heterozygous positive for two different genetic mutations of ABCB4 (one pathologic, and another of undetermined significance), thereby confirming the diagnosis of PFIC Type 3. The patient underwent liver transplant with subsequent resolution of his liver disease.
Discussion: PFIC Type 3 is caused by a defect in the ABCB4 gene on chromosome 7 which transcribes the MDR3 protein. MDR3 is responsible for biliary excretion at the hepatocyte membrane. The clinical phenotype varies from neonatal cholestasis and cirrhosis in young adults. Diagnosis can be tricky and requires detailed serological evaluation with genetic analysis for confirmation. Most patients have homozygous pathological mutation of ABCB4. However, less than 10% of patients (including ours) have only pathological mutations. UDCA is the first line of treatment with transplant being curative. Clinicians must be aware of this condition as early treatment and transplantation can prevent unnecessary morbidity and reduce mortality.
Disclosures:
Nimish Thakral indicated no relevant financial relationships.
Kishore Karri indicated no relevant financial relationships.
Jerapas Thongpiya indicated no relevant financial relationships.
Nimish Thakral, MD1, Kishore Karri, MBBS, MD1, Jerapas Thongpiya, MD2. P3079 - Progressive Familial Intrahepatic Cholestasis: A Histological Conundrum, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
