Monday Poster Session
Category: Liver
P3082 - Congenital Intrahepatic Portosystemic Shunt: A Rare Cause of Altered Mental Status
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Carla Barberan Parraga, MD
Maimonides Medical Center
New York, NY
Presenting Author(s)
Award: Presidential Poster Award
Carla Barberan Parraga, MD1, Diana Cheung, DO2, Tanuj Chokshi, DO3, Neha Sharma, MBBS, MD4, Prem Shankar, MD2, Muhammad Ali Chaudhry, MBBS2, Dmitriy Zadushlivy, MD2, Dmitri Igonkin, MD2, Yuriy Tsirlin, MD2
1Maimonides Medical Center, New York, NY; 2Maimonides Medical Center, Brooklyn, NY; 3Maimonides Medical Center, Clifton, NJ; 4Maimonides Health, Brooklyn, NY
Introduction: Intrahepatic portosystemic shunts (IHPSS) are rare vascular communications between the portal veins and the systemic circulation that bypass liver metabolism, leading to hyperammonemia and hepatic encephalopathy. If congenital, it can have variable symptomatology from hepatic encephalopathy to asymptomatic until events like gastrointestinal bleeding or constipation can trigger symptomatology, usually in adult age. Since the most common presentation is altered mental status due to encephalopathy, patients may be wrongly diagnosed with a psychiatric or neurologic disorder.
Case Description/Methods: We present a case of a 77-year-old man with a past medical history of heart failure with reduced ejection fraction (HFrEF), coronary artery bypass surgery in 1995, peptic ulcer disease, hyperthyroidism, hypertension, hyperlipidemia, and Gilbert’s syndrome, who initially presented with cognitive decline, sleep cycle abnormalities and agitation. Initial evaluation with toxicology screen, neurology and psychiatry evaluations, brain CT and MRI ruled out neurologic, psychiatric and toxic causes of altered mental. Further workup was significant for Total bilirubin (TB) of 3.1 mg/dL, Direct bilirubin (DB) of 1.3 mg/dL, normal liver enzymes, and hyperammonemia of 265 umol/L, with a normal-appearing liver on an ultrasound. Despite the patient being on treatment with lactulose, the patient continued to worsen with recurrent admissions for altered mental status, jaundice, and asterixis. Extensive workup was performed to evaluate for chronic liver disease, including serology for infectious and autoimmune conditions and tumor markers, all resulting negative or unremarkable. An MRI of the Abdomen with IV contrast was performed, describing a noncirrhotic liver contour with a 2.1 cm enhancing lesion in the right hepatic lobe, which is likely an intrahepatic portosystemic shunt. The patient was treated by Interventional Radiology with transcatheter embolization via the transhepatic portal vein, resulting in an fairly rapid improvement in the patient’s mental status and did require any further treatment with lactulose.
Discussion: This case highlights the importance of considering rare causes of hepatic abnormalities in patients with unexplained hyperammonemia and encephalopathy when the initial workup of common causes is inconclusive, especially without history or findings of cirrhosis. Early recognition and appropriate management can lead to improved outcomes and quality of life.
Disclosures:
Carla Barberan Parraga, MD1, Diana Cheung, DO2, Tanuj Chokshi, DO3, Neha Sharma, MBBS, MD4, Prem Shankar, MD2, Muhammad Ali Chaudhry, MBBS2, Dmitriy Zadushlivy, MD2, Dmitri Igonkin, MD2, Yuriy Tsirlin, MD2. P3082 - Congenital Intrahepatic Portosystemic Shunt: A Rare Cause of Altered Mental Status, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Carla Barberan Parraga, MD1, Diana Cheung, DO2, Tanuj Chokshi, DO3, Neha Sharma, MBBS, MD4, Prem Shankar, MD2, Muhammad Ali Chaudhry, MBBS2, Dmitriy Zadushlivy, MD2, Dmitri Igonkin, MD2, Yuriy Tsirlin, MD2
1Maimonides Medical Center, New York, NY; 2Maimonides Medical Center, Brooklyn, NY; 3Maimonides Medical Center, Clifton, NJ; 4Maimonides Health, Brooklyn, NY
Introduction: Intrahepatic portosystemic shunts (IHPSS) are rare vascular communications between the portal veins and the systemic circulation that bypass liver metabolism, leading to hyperammonemia and hepatic encephalopathy. If congenital, it can have variable symptomatology from hepatic encephalopathy to asymptomatic until events like gastrointestinal bleeding or constipation can trigger symptomatology, usually in adult age. Since the most common presentation is altered mental status due to encephalopathy, patients may be wrongly diagnosed with a psychiatric or neurologic disorder.
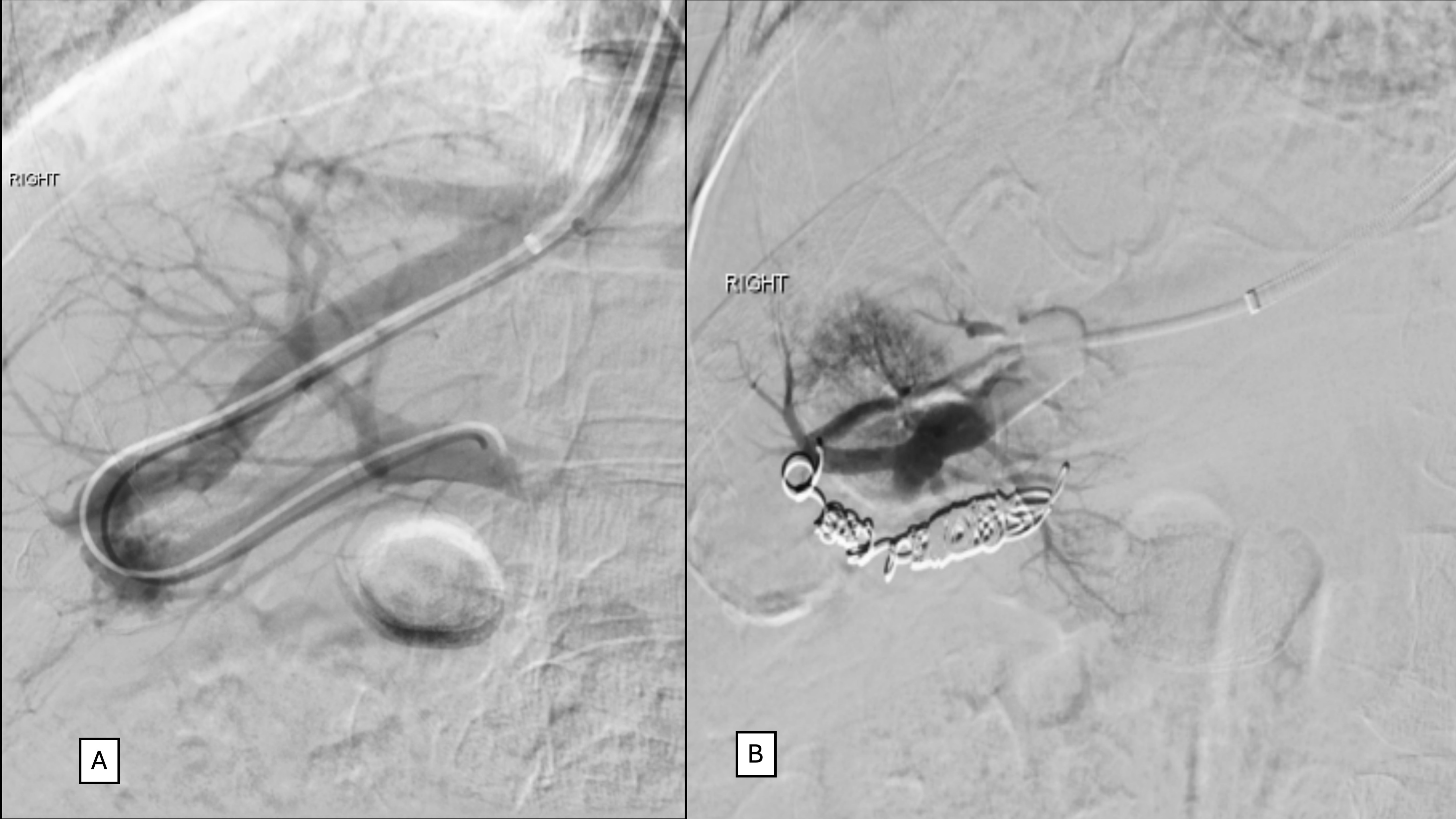
Case Description/Methods: We present a case of a 77-year-old man with a past medical history of heart failure with reduced ejection fraction (HFrEF), coronary artery bypass surgery in 1995, peptic ulcer disease, hyperthyroidism, hypertension, hyperlipidemia, and Gilbert’s syndrome, who initially presented with cognitive decline, sleep cycle abnormalities and agitation. Initial evaluation with toxicology screen, neurology and psychiatry evaluations, brain CT and MRI ruled out neurologic, psychiatric and toxic causes of altered mental. Further workup was significant for Total bilirubin (TB) of 3.1 mg/dL, Direct bilirubin (DB) of 1.3 mg/dL, normal liver enzymes, and hyperammonemia of 265 umol/L, with a normal-appearing liver on an ultrasound. Despite the patient being on treatment with lactulose, the patient continued to worsen with recurrent admissions for altered mental status, jaundice, and asterixis. Extensive workup was performed to evaluate for chronic liver disease, including serology for infectious and autoimmune conditions and tumor markers, all resulting negative or unremarkable. An MRI of the Abdomen with IV contrast was performed, describing a noncirrhotic liver contour with a 2.1 cm enhancing lesion in the right hepatic lobe, which is likely an intrahepatic portosystemic shunt. The patient was treated by Interventional Radiology with transcatheter embolization via the transhepatic portal vein, resulting in an fairly rapid improvement in the patient’s mental status and did require any further treatment with lactulose.
Discussion: This case highlights the importance of considering rare causes of hepatic abnormalities in patients with unexplained hyperammonemia and encephalopathy when the initial workup of common causes is inconclusive, especially without history or findings of cirrhosis. Early recognition and appropriate management can lead to improved outcomes and quality of life.
Figure: Imaging the intrahepatic portosystemic shunt pre (A) and post (B) embolization with coils. Image A, Highlights the connection between the hepatic vein and the portal vein.
Disclosures:
Carla Barberan Parraga indicated no relevant financial relationships.
Diana Cheung indicated no relevant financial relationships.
Tanuj Chokshi indicated no relevant financial relationships.
Neha Sharma indicated no relevant financial relationships.
Prem Shankar indicated no relevant financial relationships.
Muhammad Ali Chaudhry indicated no relevant financial relationships.
Dmitriy Zadushlivy indicated no relevant financial relationships.
Dmitri Igonkin indicated no relevant financial relationships.
Yuriy Tsirlin indicated no relevant financial relationships.
Carla Barberan Parraga, MD1, Diana Cheung, DO2, Tanuj Chokshi, DO3, Neha Sharma, MBBS, MD4, Prem Shankar, MD2, Muhammad Ali Chaudhry, MBBS2, Dmitriy Zadushlivy, MD2, Dmitri Igonkin, MD2, Yuriy Tsirlin, MD2. P3082 - Congenital Intrahepatic Portosystemic Shunt: A Rare Cause of Altered Mental Status, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.


