Monday Poster Session
Category: Liver
P3084 - Obliterative Portal Venopathy: An Unusual Case of Liver Fibrosis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Carla Barberan Parraga, MD
Maimonides Medical Center
New York, NY
Presenting Author(s)
Carla Barberan Parraga, MD1, Tanuj Chokshi, DO2, Syed Mujtaba Baqir, MD3, Jimyeong Son, NP4, Leandro Sierra, MD5, Meredith E. Pittman, MD3, James Park, MD6
1Maimonides Medical Center, New York, NY; 2Maimonides Medical Center, Clifton, NJ; 3Maimonides Medical Center, Brooklyn, NY; 4Maimonides Medical Center, New Rochelle, NY; 5Cleveland Clinic Foundation, Cleveland, OH; 6Maimonides Medical Center, Manhasset, NY
Introduction: Obliterative portal venopathy (OPV) is a rare cause of portal hypertension in the absence of cirrhosis. It involves a pathologic obliteration of the intrahepatic portal venous branches, leading to increased splanchnic blood flow. It typically manifests with variceal bleeding in young patients without evidence of liver insufficiency or cirrhosis. Differentiation from cirrhosis is paramount since major differences exist in managing both pathologies. OPV is diagnosed by liver biopsy. Since it is a rare condition, at times, it can be wrongly categorized as cryptogenic cirrhosis. There is no established cause of OPV, although it has been associated with HIV infection, Schistosomiasis, prothrombotic states, and medications like Didanosine and Azathioprine.
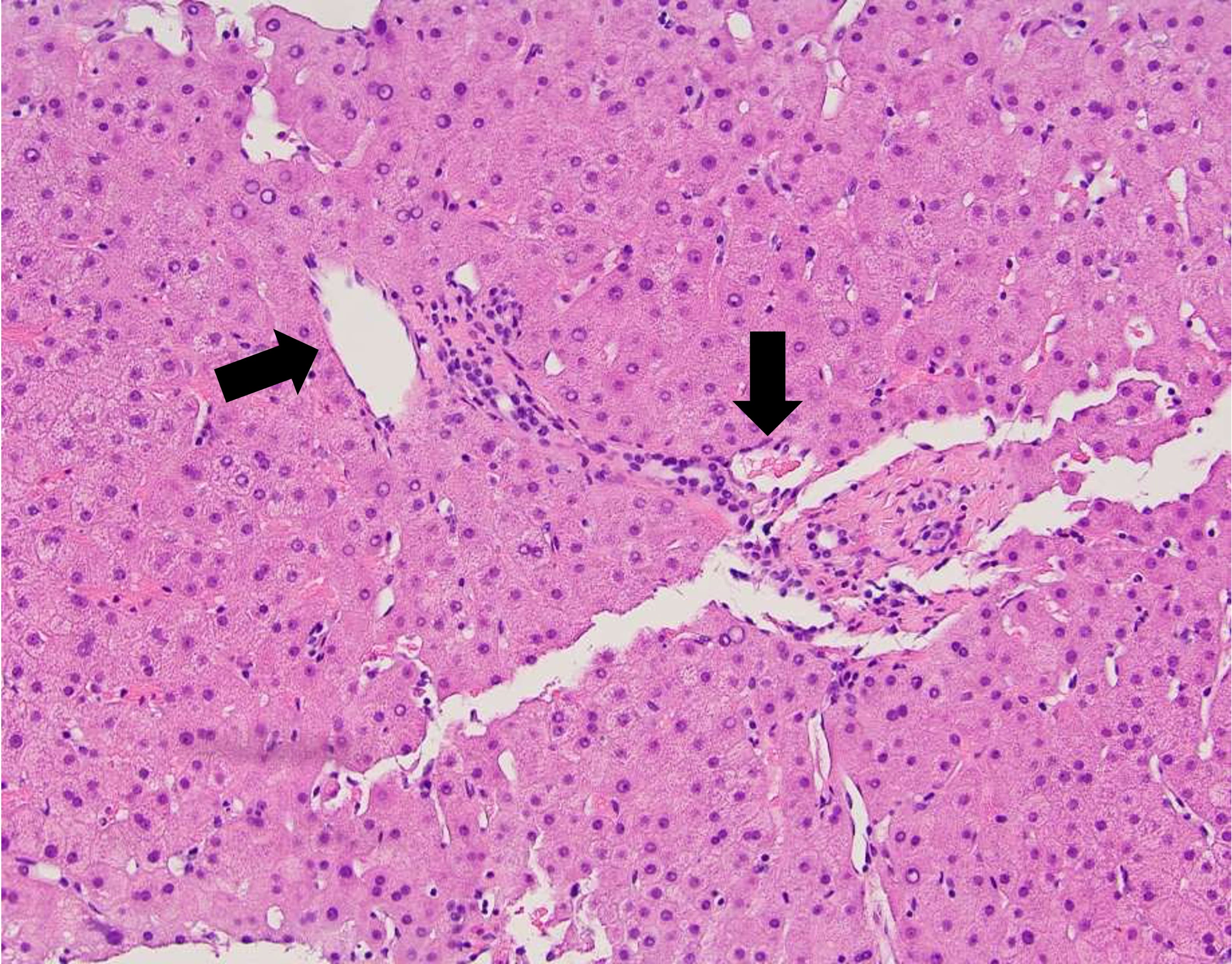
Case Description/Methods: We describe a case of a 68-year-old woman referred to the Gastroenterology clinic for liver fibrosis evaluation due to persistent, mildly elevated liver enzymes. Elastography indicated advanced fibrosis (F3-F4), and prior esophagogastroduodenoscopy revealed no varices. The patient denied symptoms and reported no use of herbal supplements, multivitamins, new medications, alcohol, tobacco, or illicit drugs. Further workup showed mild elevation in liver enzymes (AST 42 IU/L, ALT 43 IU/L, and ALP 121 IU/L) and moderate-severe fibrosis on elastography (1.84 m/s stiffness velocity). MRI of the abdomen with contrast highlighted a nodular liver contour suggestive of cirrhosis without additional cirrhotic features or liver lesions. Test for chronic liver diseases, including viral hepatitis, autoantibodies, and tumor markers, were within normal range, except for elevated ANA antibody 1:1280 and IgG 1733, initially raising suspicion of autoimmune hepatitis or metabolic-associated steatotic liver disease. However, due to concerns about corticosteroid therapy, a liver biopsy was pursued, showing histologic patterns consistent with idiopathic, non-cirrhotic portal hypertension. Further evaluations for OPV, including parasite testing, additional medication and supplement assessment, and HIV testing, did not yield significant findings.
Discussion: This case highlights the importance of considering OPV in the differential diagnosis of liver fibrosis, as inappropriate management can be detrimental to this pathology. Management of OPV is mainly symptomatic treatment of upper gastrointestinal bleeds. In OPV, liver function tests remain normal until later in the disease course. Otherwise, it has a good prognosis and survival rates.
Disclosures:
Carla Barberan Parraga, MD1, Tanuj Chokshi, DO2, Syed Mujtaba Baqir, MD3, Jimyeong Son, NP4, Leandro Sierra, MD5, Meredith E. Pittman, MD3, James Park, MD6. P3084 - Obliterative Portal Venopathy: An Unusual Case of Liver Fibrosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Maimonides Medical Center, New York, NY; 2Maimonides Medical Center, Clifton, NJ; 3Maimonides Medical Center, Brooklyn, NY; 4Maimonides Medical Center, New Rochelle, NY; 5Cleveland Clinic Foundation, Cleveland, OH; 6Maimonides Medical Center, Manhasset, NY
Introduction: Obliterative portal venopathy (OPV) is a rare cause of portal hypertension in the absence of cirrhosis. It involves a pathologic obliteration of the intrahepatic portal venous branches, leading to increased splanchnic blood flow. It typically manifests with variceal bleeding in young patients without evidence of liver insufficiency or cirrhosis. Differentiation from cirrhosis is paramount since major differences exist in managing both pathologies. OPV is diagnosed by liver biopsy. Since it is a rare condition, at times, it can be wrongly categorized as cryptogenic cirrhosis. There is no established cause of OPV, although it has been associated with HIV infection, Schistosomiasis, prothrombotic states, and medications like Didanosine and Azathioprine.
Case Description/Methods: We describe a case of a 68-year-old woman referred to the Gastroenterology clinic for liver fibrosis evaluation due to persistent, mildly elevated liver enzymes. Elastography indicated advanced fibrosis (F3-F4), and prior esophagogastroduodenoscopy revealed no varices. The patient denied symptoms and reported no use of herbal supplements, multivitamins, new medications, alcohol, tobacco, or illicit drugs. Further workup showed mild elevation in liver enzymes (AST 42 IU/L, ALT 43 IU/L, and ALP 121 IU/L) and moderate-severe fibrosis on elastography (1.84 m/s stiffness velocity). MRI of the abdomen with contrast highlighted a nodular liver contour suggestive of cirrhosis without additional cirrhotic features or liver lesions. Test for chronic liver diseases, including viral hepatitis, autoantibodies, and tumor markers, were within normal range, except for elevated ANA antibody 1:1280 and IgG 1733, initially raising suspicion of autoimmune hepatitis or metabolic-associated steatotic liver disease. However, due to concerns about corticosteroid therapy, a liver biopsy was pursued, showing histologic patterns consistent with idiopathic, non-cirrhotic portal hypertension. Further evaluations for OPV, including parasite testing, additional medication and supplement assessment, and HIV testing, did not yield significant findings.
Discussion: This case highlights the importance of considering OPV in the differential diagnosis of liver fibrosis, as inappropriate management can be detrimental to this pathology. Management of OPV is mainly symptomatic treatment of upper gastrointestinal bleeds. In OPV, liver function tests remain normal until later in the disease course. Otherwise, it has a good prognosis and survival rates.
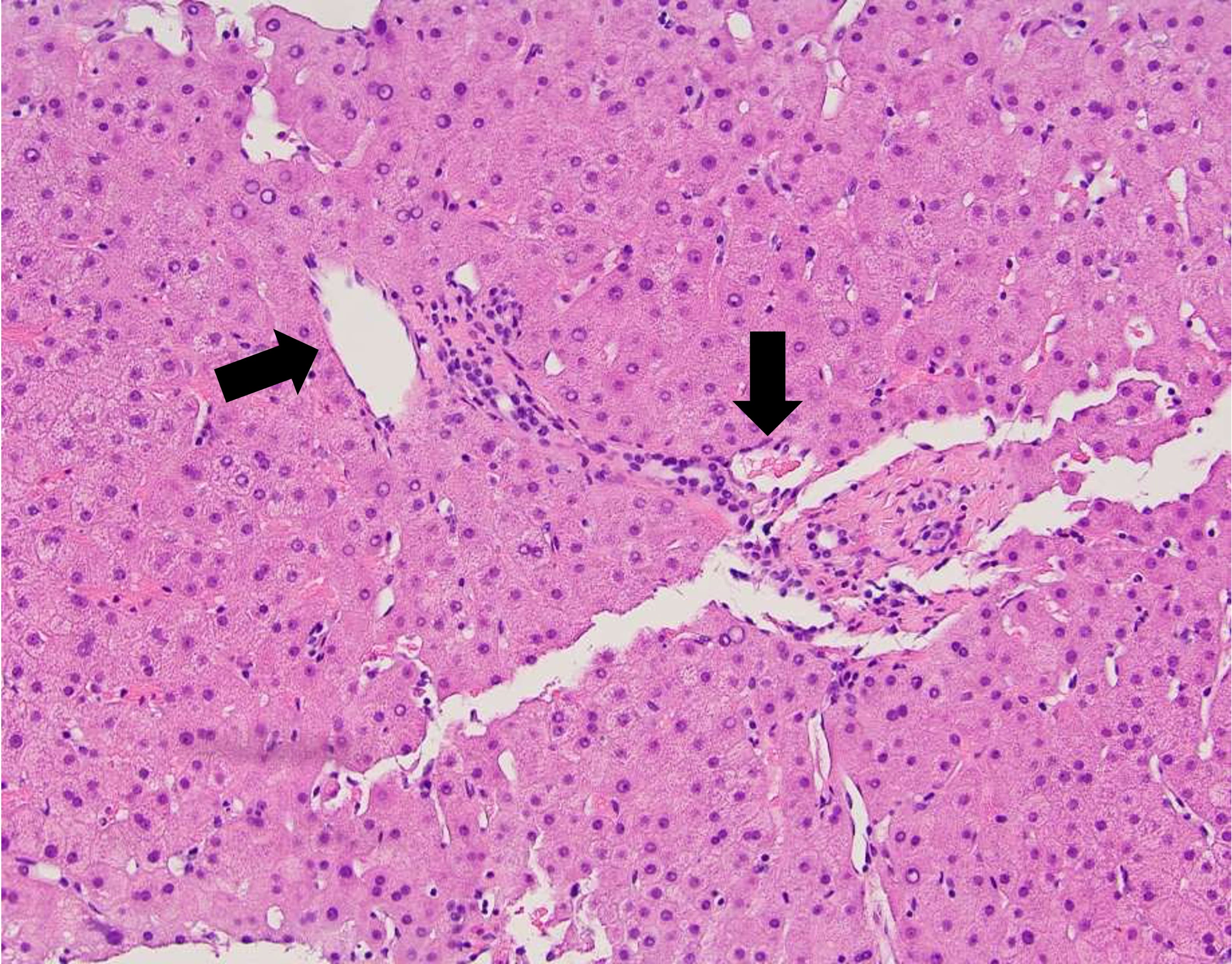
Figure: Liver biopsy H&E stain. Non-inflamed portal tracts with veins that herniate from the portal tracts into surrounding hepatocytes.
Disclosures:
Carla Barberan Parraga indicated no relevant financial relationships.
Tanuj Chokshi indicated no relevant financial relationships.
Syed Mujtaba Baqir indicated no relevant financial relationships.
Jimyeong Son indicated no relevant financial relationships.
Leandro Sierra indicated no relevant financial relationships.
Meredith Pittman indicated no relevant financial relationships.
James Park indicated no relevant financial relationships.
Carla Barberan Parraga, MD1, Tanuj Chokshi, DO2, Syed Mujtaba Baqir, MD3, Jimyeong Son, NP4, Leandro Sierra, MD5, Meredith E. Pittman, MD3, James Park, MD6. P3084 - Obliterative Portal Venopathy: An Unusual Case of Liver Fibrosis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
