Monday Poster Session
Category: Liver
P3087 - A Case of Pylephlebitis in the Absence of Clear Intra-Abdominal Suppurative Processes or Hyper-Coagulable State
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Grace Ann Thomas, MD, MS
University of Tennessee Health Science Center
Memphis, TN
Presenting Author(s)
Grace Ann Thomas, MD, MS1, Tyson Amundsen, MD, BA2, Mansour Parsi, MD, MPH, MBA.3
1University of Tennessee Health Science Center, Memphis, TN; 2University of Tennessee Health Science Center, Bartlett, TN; 3University of Tennessee College of Medicine, Memphis, TN
Introduction: Pylephlebitis is an infective thrombophlebitis of the portal vein and a rare complication of intra-abdominal or pelvic infections, typically appendicitis or diverticulitis. We present a case of pylephlebitis in the absence of clear intra-abdominal suppurative processes or hypercoagulable state.
Case Description/Methods: A 63-year-old man with history of hyperlipidemia and left portal vein thrombosis presents with a week of chest and abdominal pain. He was tachycardic, hypotensive, and tachypneic. WBC was 40K, ALP 295, AST/ALT 248/210. He was admitted three weeks prior and was found to have portal vein thrombosis on CT Abdomen and Pelvis with contrast. He had no history of stroke, DVT, MI, PE, clotting or bleeding disorders. His symptoms resolved with initiation of heparin and was discharged on direct oral anticoagulation.
Repeat CT showed a complete opacification of right portal vein branches and many liver hypodensities. Patient was taken for portal vein thrombectomy, yielding frank purulent material, consistent with pylephlebitis. There was a posterior liver abscess which drained 20 mL of thick purulent fluid with cultures positive for Strep. constellatus, parvomonas micra, and coagulase negative staph. Blood cultures were positive for Strep. constellatus.
He was discharged to rehab, and a week later, repeat CT showed many intrahepatic fluid collections, extending into the diaphragm. Patient had no change in symptoms. IR upsized the hepatic drain, yielding necrotic material. Thoracic surgery took the patient for VATS. Diffuse adhesions were noted but the diaphragm could not be visualized because of a phlegmon. Surgical oncology took the patient for robotic right liver lobe resection. Intra-operative cultures showed gram negative rods and candida. Patient was discharged with one month of Levaquin, flagyl, and fluconazole with improvement of symptoms.
Discussion: This is an example of septic pylephlebitis without an obvious source intra-abdominal infection. Fever is the most common presenting symptom of pylephlebitis, and this patient was afebrile. Prevalent causes of pylephlebitis include diverticulitis, appendicitis, or contiguous infection such as cholangitis or cholecystitis. While a hepatic abscess was found and drained shortly after initial thrombectomy, it is difficult to assess whether this is a cause of pylephlebitis or a consequence. Malignancy and thrombophilia workup were unremarkable. Bone marrow aspirate was concerning for myelodysplastic syndrome but were ultimately inconclusive.
Disclosures:
Grace Ann Thomas, MD, MS1, Tyson Amundsen, MD, BA2, Mansour Parsi, MD, MPH, MBA.3. P3087 - A Case of Pylephlebitis in the Absence of Clear Intra-Abdominal Suppurative Processes or Hyper-Coagulable State, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Tennessee Health Science Center, Memphis, TN; 2University of Tennessee Health Science Center, Bartlett, TN; 3University of Tennessee College of Medicine, Memphis, TN
Introduction: Pylephlebitis is an infective thrombophlebitis of the portal vein and a rare complication of intra-abdominal or pelvic infections, typically appendicitis or diverticulitis. We present a case of pylephlebitis in the absence of clear intra-abdominal suppurative processes or hypercoagulable state.
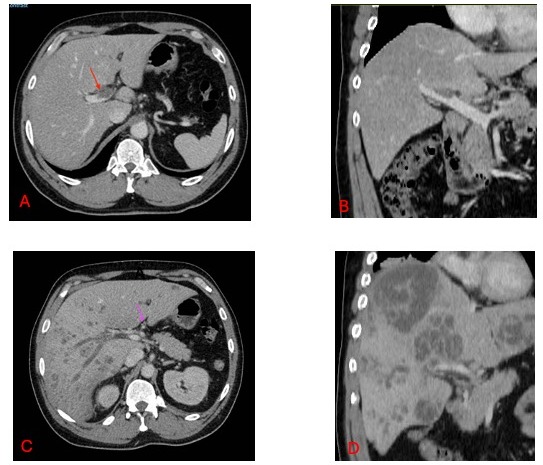
Case Description/Methods: A 63-year-old man with history of hyperlipidemia and left portal vein thrombosis presents with a week of chest and abdominal pain. He was tachycardic, hypotensive, and tachypneic. WBC was 40K, ALP 295, AST/ALT 248/210. He was admitted three weeks prior and was found to have portal vein thrombosis on CT Abdomen and Pelvis with contrast. He had no history of stroke, DVT, MI, PE, clotting or bleeding disorders. His symptoms resolved with initiation of heparin and was discharged on direct oral anticoagulation.
Repeat CT showed a complete opacification of right portal vein branches and many liver hypodensities. Patient was taken for portal vein thrombectomy, yielding frank purulent material, consistent with pylephlebitis. There was a posterior liver abscess which drained 20 mL of thick purulent fluid with cultures positive for Strep. constellatus, parvomonas micra, and coagulase negative staph. Blood cultures were positive for Strep. constellatus.
He was discharged to rehab, and a week later, repeat CT showed many intrahepatic fluid collections, extending into the diaphragm. Patient had no change in symptoms. IR upsized the hepatic drain, yielding necrotic material. Thoracic surgery took the patient for VATS. Diffuse adhesions were noted but the diaphragm could not be visualized because of a phlegmon. Surgical oncology took the patient for robotic right liver lobe resection. Intra-operative cultures showed gram negative rods and candida. Patient was discharged with one month of Levaquin, flagyl, and fluconazole with improvement of symptoms.
Discussion: This is an example of septic pylephlebitis without an obvious source intra-abdominal infection. Fever is the most common presenting symptom of pylephlebitis, and this patient was afebrile. Prevalent causes of pylephlebitis include diverticulitis, appendicitis, or contiguous infection such as cholangitis or cholecystitis. While a hepatic abscess was found and drained shortly after initial thrombectomy, it is difficult to assess whether this is a cause of pylephlebitis or a consequence. Malignancy and thrombophilia workup were unremarkable. Bone marrow aspirate was concerning for myelodysplastic syndrome but were ultimately inconclusive.
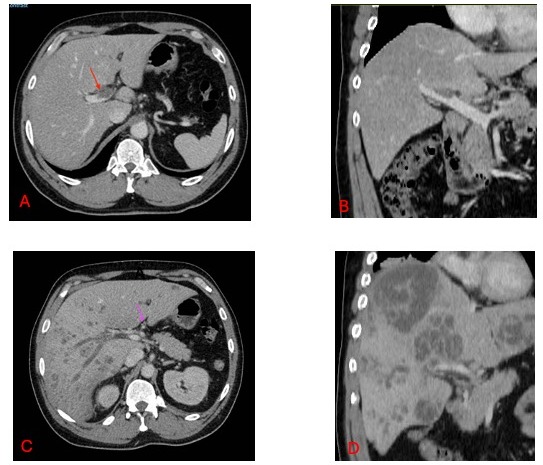
Figure: Figures A and B represent the CT abdomen with contrast that was obtained on our patient's initial presentation, demonstrating portal vein thrombosis.
Figures C and D represent CT Abdomen with contrast obtained three weeks after initial presentation, demonstrating portal vein thrombosis and multiple hepatic infarcts.
Figures C and D represent CT Abdomen with contrast obtained three weeks after initial presentation, demonstrating portal vein thrombosis and multiple hepatic infarcts.
Disclosures:
Grace Ann Thomas indicated no relevant financial relationships.
Tyson Amundsen indicated no relevant financial relationships.
Mansour Parsi indicated no relevant financial relationships.
Grace Ann Thomas, MD, MS1, Tyson Amundsen, MD, BA2, Mansour Parsi, MD, MPH, MBA.3. P3087 - A Case of Pylephlebitis in the Absence of Clear Intra-Abdominal Suppurative Processes or Hyper-Coagulable State, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
