Monday Poster Session
Category: Liver
P3121 - The Yellow Submarine: Rare Case of a Patient With Benign Intrahepatic Cholestasis With a Pathogenic Genetic Variant Consistent With Progressive Familial Intrahepatic Cholestasis
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- SC
Subin Chirayath, DO
St. Luke's University Health Network
Allentown, PA
Presenting Author(s)
Subin Chirayath, DO1, Li Ge, MD2, Vishal Patel, MD2, Ashley Tran, MD2
1St. Luke's University Health Network, Allentown, PA; 2St. Luke's University Health Network, Bethlehem, PA
Introduction: Benign recurrent intrahepatic cholestasis (BRIC) is a benign condition characterized by recurrent episodes of jaundice and cholestatic pruritus in patients during stress, infection or oral contraceptive use (OCP). BRIC-1 is caused by a mutation in the ATP8B1 gene which causes FIC1 deficiency. BRIC-1 shares the same genetic mutation as progressive familial intrahepatic cholestasis (PFIC-1) which leads to early development of cirrhosis. We present a case of a patient diagnosed with BRIC who had a mild disease phenotype despite having two pathogenic variants in the ATP8B1 gene.
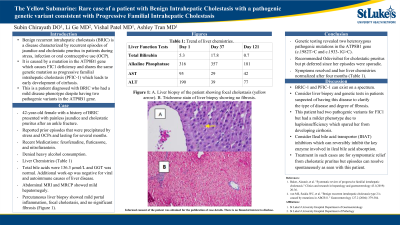
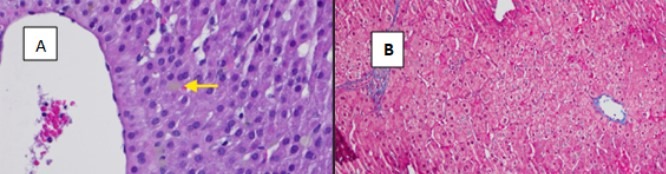
Case Description/Methods: 42-year-old female with a history of BRIC presented with painless jaundice and cholestatic pruritus after an ankle fracture. She reported prior episodes precipitated by stress and OCPs and lasting for several months. Her medications included fexofenadine, fluticasone, and nitrofurantoin. She denied heavy alcohol consumption, recreational drug use, high-risk sexual behaviors, and medication changes. Her physical exam showed scleral icterus and jaundice but was otherwise unremarkable. Labs revealed ALT 190 U/L, AST 95 U/L, alkaline phosphatase 316, and total bilirubin 5.3 mg/dL. Her total bile acids were 136.3 μmol/L and GGT was normal. Additional work-up was negative for viral and autoimmune and liver diseases. Abdominal MRI and MRCP showed mild hepatomegaly but no biliary dilatation or obstruction. She had a percutaneous liver biopsy which showed mild portal inflammation, focal cholestasis, and no significant fibrosis (Figure 1). Genetic testing revealed two heterozygous pathogenic mutations in the ATP8B1 gene (c.1982T >C and c.1933-1G >C). She was recommended Odevixibat for cholestatic pruritus but deferred since her episodes were sporadic. Her symptoms resolved and her liver chemistries normalized after four months (Table 2).
Discussion: BRIC-1 and PFIC-1 exist on opposite ends of the spectrum for FIC1 disease. The clinical phenotype can range in severity from mild, recurrent disease to end-staged liver disease requiring biliary diversion or liver transplantation. The development of PFIC-1 in patients with BRIC has been reported. Therefore, liver biopsy and genetic testing should be considered in all patients with unexplained intrahepatic cholestasis. Our patient had two pathogenic variants for FIC1 but had a milder phenotype due to haploinsufficiency. Ileal bile acid transporter (IBAT) inhibitors should be considered in such cases for cholestatic pruritus and warrants further investigation.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Subin Chirayath, DO1, Li Ge, MD2, Vishal Patel, MD2, Ashley Tran, MD2. P3121 - The Yellow Submarine: Rare Case of a Patient With Benign Intrahepatic Cholestasis With a Pathogenic Genetic Variant Consistent With Progressive Familial Intrahepatic Cholestasis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1St. Luke's University Health Network, Allentown, PA; 2St. Luke's University Health Network, Bethlehem, PA
Introduction: Benign recurrent intrahepatic cholestasis (BRIC) is a benign condition characterized by recurrent episodes of jaundice and cholestatic pruritus in patients during stress, infection or oral contraceptive use (OCP). BRIC-1 is caused by a mutation in the ATP8B1 gene which causes FIC1 deficiency. BRIC-1 shares the same genetic mutation as progressive familial intrahepatic cholestasis (PFIC-1) which leads to early development of cirrhosis. We present a case of a patient diagnosed with BRIC who had a mild disease phenotype despite having two pathogenic variants in the ATP8B1 gene.
Case Description/Methods: 42-year-old female with a history of BRIC presented with painless jaundice and cholestatic pruritus after an ankle fracture. She reported prior episodes precipitated by stress and OCPs and lasting for several months. Her medications included fexofenadine, fluticasone, and nitrofurantoin. She denied heavy alcohol consumption, recreational drug use, high-risk sexual behaviors, and medication changes. Her physical exam showed scleral icterus and jaundice but was otherwise unremarkable. Labs revealed ALT 190 U/L, AST 95 U/L, alkaline phosphatase 316, and total bilirubin 5.3 mg/dL. Her total bile acids were 136.3 μmol/L and GGT was normal. Additional work-up was negative for viral and autoimmune and liver diseases. Abdominal MRI and MRCP showed mild hepatomegaly but no biliary dilatation or obstruction. She had a percutaneous liver biopsy which showed mild portal inflammation, focal cholestasis, and no significant fibrosis (Figure 1). Genetic testing revealed two heterozygous pathogenic mutations in the ATP8B1 gene (c.1982T >C and c.1933-1G >C). She was recommended Odevixibat for cholestatic pruritus but deferred since her episodes were sporadic. Her symptoms resolved and her liver chemistries normalized after four months (Table 2).
Discussion: BRIC-1 and PFIC-1 exist on opposite ends of the spectrum for FIC1 disease. The clinical phenotype can range in severity from mild, recurrent disease to end-staged liver disease requiring biliary diversion or liver transplantation. The development of PFIC-1 in patients with BRIC has been reported. Therefore, liver biopsy and genetic testing should be considered in all patients with unexplained intrahepatic cholestasis. Our patient had two pathogenic variants for FIC1 but had a milder phenotype due to haploinsufficiency. Ileal bile acid transporter (IBAT) inhibitors should be considered in such cases for cholestatic pruritus and warrants further investigation.
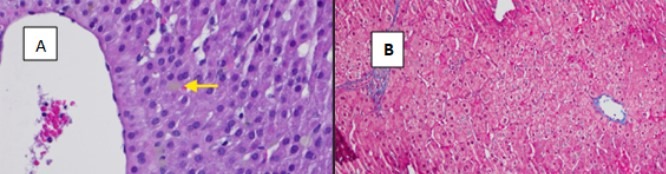
Figure: Figure 1: A. Liver biopsy of the patient showing focal cholestasis (yellow arrow). B. Trichrome stain of liver biopsy showing no fibrosis.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Subin Chirayath indicated no relevant financial relationships.
Li Ge indicated no relevant financial relationships.
Vishal Patel indicated no relevant financial relationships.
Ashley Tran indicated no relevant financial relationships.
Subin Chirayath, DO1, Li Ge, MD2, Vishal Patel, MD2, Ashley Tran, MD2. P3121 - The Yellow Submarine: Rare Case of a Patient With Benign Intrahepatic Cholestasis With a Pathogenic Genetic Variant Consistent With Progressive Familial Intrahepatic Cholestasis, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
