Monday Poster Session
Category: Liver
P3124 - Veno-Occlusive Disease as a Rare Complication of Ipilimumab and Nivolumab
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- WB
William Bigelow, MD
University of Virginia
Charlottesville, VA
Presenting Author(s)
William Bigelow, MD1, Zachary Henry, MD2, Brian J. Wentworth, MD, MS2, Mary Sullivan, MD1
1University of Virginia, Charlottesville, VA; 2University of Virginia Medical Center, Charlottesville, VA
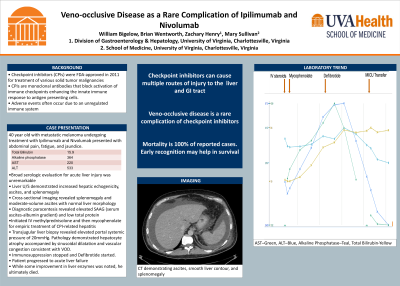
Introduction: Checkpoint inhibitors (CPIs) were approved to treat various solid tumor malignancies in 2011. They function as monoclonal antibodies that block activation of immune checkpoints allowing enhancement of the innate immune response to antigen presenting cells and overall tumor burden. While monumental for increased survival in many malignancies, adverse events due to an unregulated immune system occur often. We describe a rare case of immune CPI-induced veno-occlusive disease (VOD) leading to acute liver failure.
Case Description/Methods: A 40-year-old male with metastatic melanoma managed with ipilimumab and nivolumab presented with abdominal pain, fatigue, and jaundice. Dual checkpoint inhibitor therapy had been initiated three months prior to admission. His total bilirubin was 15.9, alkaline phosphatase 364, AST 220, and ALT 533. A broad serologic evaluation of acute liver injury was obtained and unremarkable for infectious, autoimmune, and inherited metabolic disease. A liver ultrasound demonstrated increased hepatic echogenicity, ascites, and splenomegaly. Subsequent cross-sectional imaging revealed splenomegaly and moderate-volume ascites with normal liver morphology. On diagnostic paracentesis, the serum ascites-albumin gradient was elevated and total protein was low consistent with portal hypertension from hepatic dysfunction. He was started on intravenous methylprednisolone and then mycophenolate for empiric CPI-related hepatitis as his bilirubin and liver enzymes continued to trend upward. A transjugular liver biopsy revealed an elevated portal systemic gradient of 20mmHg. Pathology demonstrated hepatocyte atrophy accompanied by sinusoidal dilatation and vascular congestion consistent with VOD. Immunosuppression was stopped and defibrotide was initiated. The patient proceeded to develop encephalopathy and coagulopathy (INR of 2.5), thus meeting criteria for progression to acute liver failure. Though he demonstrated some mild improvement in his liver enzymes over the subsequent days, he ultimately died.
Discussion: Checkpoint inhibitors are increasingly being developed and utilized for additional solid tumor malignancies. While CPI-related hepatitis is commonly encountered, clinicians should be aware of VOD as an exceedingly rare but potentially fatal adverse event. There have been a few case reports of VOD in relation to nivolumab and cemiplimab, with 100% mortality related to the development of liver failure. Early recognition and treatment for VOD is critical for potential survival.
Disclosures:
William Bigelow, MD1, Zachary Henry, MD2, Brian J. Wentworth, MD, MS2, Mary Sullivan, MD1. P3124 - Veno-Occlusive Disease as a Rare Complication of Ipilimumab and Nivolumab, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Virginia, Charlottesville, VA; 2University of Virginia Medical Center, Charlottesville, VA
Introduction: Checkpoint inhibitors (CPIs) were approved to treat various solid tumor malignancies in 2011. They function as monoclonal antibodies that block activation of immune checkpoints allowing enhancement of the innate immune response to antigen presenting cells and overall tumor burden. While monumental for increased survival in many malignancies, adverse events due to an unregulated immune system occur often. We describe a rare case of immune CPI-induced veno-occlusive disease (VOD) leading to acute liver failure.
Case Description/Methods: A 40-year-old male with metastatic melanoma managed with ipilimumab and nivolumab presented with abdominal pain, fatigue, and jaundice. Dual checkpoint inhibitor therapy had been initiated three months prior to admission. His total bilirubin was 15.9, alkaline phosphatase 364, AST 220, and ALT 533. A broad serologic evaluation of acute liver injury was obtained and unremarkable for infectious, autoimmune, and inherited metabolic disease. A liver ultrasound demonstrated increased hepatic echogenicity, ascites, and splenomegaly. Subsequent cross-sectional imaging revealed splenomegaly and moderate-volume ascites with normal liver morphology. On diagnostic paracentesis, the serum ascites-albumin gradient was elevated and total protein was low consistent with portal hypertension from hepatic dysfunction. He was started on intravenous methylprednisolone and then mycophenolate for empiric CPI-related hepatitis as his bilirubin and liver enzymes continued to trend upward. A transjugular liver biopsy revealed an elevated portal systemic gradient of 20mmHg. Pathology demonstrated hepatocyte atrophy accompanied by sinusoidal dilatation and vascular congestion consistent with VOD. Immunosuppression was stopped and defibrotide was initiated. The patient proceeded to develop encephalopathy and coagulopathy (INR of 2.5), thus meeting criteria for progression to acute liver failure. Though he demonstrated some mild improvement in his liver enzymes over the subsequent days, he ultimately died.
Discussion: Checkpoint inhibitors are increasingly being developed and utilized for additional solid tumor malignancies. While CPI-related hepatitis is commonly encountered, clinicians should be aware of VOD as an exceedingly rare but potentially fatal adverse event. There have been a few case reports of VOD in relation to nivolumab and cemiplimab, with 100% mortality related to the development of liver failure. Early recognition and treatment for VOD is critical for potential survival.
Disclosures:
William Bigelow indicated no relevant financial relationships.
Zachary Henry indicated no relevant financial relationships.
Brian Wentworth indicated no relevant financial relationships.
Mary Sullivan indicated no relevant financial relationships.
William Bigelow, MD1, Zachary Henry, MD2, Brian J. Wentworth, MD, MS2, Mary Sullivan, MD1. P3124 - Veno-Occlusive Disease as a Rare Complication of Ipilimumab and Nivolumab, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

