Monday Poster Session
Category: Liver
P3126 - A Case of Auto Brewery Syndrome (ABS) Complicating Cirrhosis and Leading to Liver Transplant
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
- MK
Muhammad Taha Khan, MD
University of Oklahoma Health Sciences Center
Oklahoma City, OK
Presenting Author(s)
Taha Khan, MD1, Luke Sorensen, MD1, Ruqaiyyah Hamid, MD2, Sidra Ahsan, MD3, Abdul Oseini, MD1
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2Piedmont Columbus Regional Hospital, Columbus, GA; 3Oklahoma University Health Sciences Center, Oklahoma City, OK
Introduction: Auto-brewery syndrome (ABS) is a rarely diagnosed condition where ingested carbohydrates are converted to alcohol by fungi in the GI tract. ABS patients can develop alcohol-related complications.
There have been only a handful of case reports describing ABS. We present a case of a patient with ABS needing liver transplant due to complications of cirrhosis.
Case Description/Methods: 54-year-old man, with a history of GERD, HTN, HLD, and MASLD, presented to his PCP after a recent hospitalization for altered mental status and elevated blood alcohol levels. He strongly denied recent alcohol use and mentioned similar occurrences in the past after large meals. He reported prior alcohol use socially, drinking beer over the weekends and occasionally hard liquor.
A 24-hour glucose challenge test, conducted after alcohol cessation and an overnight fast, was positive for elevated blood alcohol levels, suggesting Auto Brewery Syndrome. Treatment included a low carbohydrate diet, alcohol abstinence, a short course of fluconazole, along with routine home breathalyzer tests.
Symptoms initially improved with compliance. However, over the next year, he developed decompensated cirrhosis, thought to be secondary to MASLD and ABS, requiring numerous hospitalizations for complications such as SBP, variceal bleed, and encephalopathy. Infectious workup did not identify a particular fungal organism as the cause of ABS. Ultimately, he underwent a successful liver transplant. Interestingly, a repeat glucose challenge test preoperatively was negative, potentially influenced by multiple rounds of anti-fungal therapy for episodes of bacteremia.
Discussion: ABS is often under-diagnosed, with medical and legal implications. It should be suspected in patients showing signs of alcohol intoxication despite minimal alcohol consumption. Risk factors include prior antibiotic use, diabetes, short bowel syndrome, MASLD, and history of IBD.
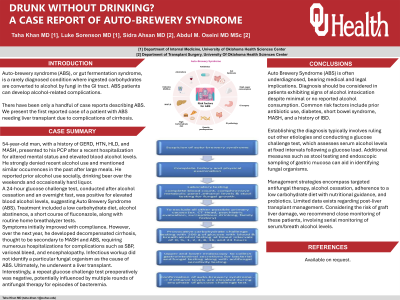
Diagnosis involves ruling out other causes and performing a glucose challenge test to assess serum alcohol levels after a glucose load (Fig 1.) Stool testing and endoscopic sampling of gastric mucosa can aid in identifying fungal organisms.
Management includes targeted anti-fungal therapy, alcohol cessation, low carbohydrate diet with nutritional guidance, and probiotics. Limited data exists on post-liver transplant care; close monitoring with serial serum/breath alcohol level checks is advised due to risk of graft liver damage.

Disclosures:
Taha Khan, MD1, Luke Sorensen, MD1, Ruqaiyyah Hamid, MD2, Sidra Ahsan, MD3, Abdul Oseini, MD1. P3126 - A Case of Auto Brewery Syndrome (ABS) Complicating Cirrhosis and Leading to Liver Transplant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1University of Oklahoma Health Sciences Center, Oklahoma City, OK; 2Piedmont Columbus Regional Hospital, Columbus, GA; 3Oklahoma University Health Sciences Center, Oklahoma City, OK
Introduction: Auto-brewery syndrome (ABS) is a rarely diagnosed condition where ingested carbohydrates are converted to alcohol by fungi in the GI tract. ABS patients can develop alcohol-related complications.
There have been only a handful of case reports describing ABS. We present a case of a patient with ABS needing liver transplant due to complications of cirrhosis.
Case Description/Methods: 54-year-old man, with a history of GERD, HTN, HLD, and MASLD, presented to his PCP after a recent hospitalization for altered mental status and elevated blood alcohol levels. He strongly denied recent alcohol use and mentioned similar occurrences in the past after large meals. He reported prior alcohol use socially, drinking beer over the weekends and occasionally hard liquor.
A 24-hour glucose challenge test, conducted after alcohol cessation and an overnight fast, was positive for elevated blood alcohol levels, suggesting Auto Brewery Syndrome. Treatment included a low carbohydrate diet, alcohol abstinence, a short course of fluconazole, along with routine home breathalyzer tests.
Symptoms initially improved with compliance. However, over the next year, he developed decompensated cirrhosis, thought to be secondary to MASLD and ABS, requiring numerous hospitalizations for complications such as SBP, variceal bleed, and encephalopathy. Infectious workup did not identify a particular fungal organism as the cause of ABS. Ultimately, he underwent a successful liver transplant. Interestingly, a repeat glucose challenge test preoperatively was negative, potentially influenced by multiple rounds of anti-fungal therapy for episodes of bacteremia.
Discussion: ABS is often under-diagnosed, with medical and legal implications. It should be suspected in patients showing signs of alcohol intoxication despite minimal alcohol consumption. Risk factors include prior antibiotic use, diabetes, short bowel syndrome, MASLD, and history of IBD.
Diagnosis involves ruling out other causes and performing a glucose challenge test to assess serum alcohol levels after a glucose load (Fig 1.) Stool testing and endoscopic sampling of gastric mucosa can aid in identifying fungal organisms.
Management includes targeted anti-fungal therapy, alcohol cessation, low carbohydrate diet with nutritional guidance, and probiotics. Limited data exists on post-liver transplant care; close monitoring with serial serum/breath alcohol level checks is advised due to risk of graft liver damage.

Figure: Fig 1. Protocol for the detection of auto-brewery syndrome described by Malik et al.
Disclosures:
Taha Khan indicated no relevant financial relationships.
Luke Sorensen indicated no relevant financial relationships.
Ruqaiyyah Hamid indicated no relevant financial relationships.
Sidra Ahsan indicated no relevant financial relationships.
Abdul Oseini indicated no relevant financial relationships.
Taha Khan, MD1, Luke Sorensen, MD1, Ruqaiyyah Hamid, MD2, Sidra Ahsan, MD3, Abdul Oseini, MD1. P3126 - A Case of Auto Brewery Syndrome (ABS) Complicating Cirrhosis and Leading to Liver Transplant, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
