Monday Poster Session
Category: Liver
P3135 - Liver Meets Legs: Unraveling Hepatic Myelopathy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
Ishan Kirti, MBBS
MedStar Union Memorial Hospital
Towson, MD
Presenting Author(s)
Award: Presidential Poster Award
Ishan Kirti, MBBS1, Matthew Lynberg, BS2, Haider A. Naqvi, MD3, Nahar Saleh, MD4
1MedStar Union Memorial Hospital, Towson, MD; 2Georgetown University School of Medicine, Washington, DC; 3MedStar Franklin Square Medical Center, Rossville, MD; 4MedStar Union Memorial Hospital, Baltimore, MD
Introduction: Hepatic myelopathy (HM) is a rare neurological complication typically associated with cirrhosis, often manifesting as progressive spastic paraparesis. It presents a diagnostic challenge due to its rarity and varied clinical presentation. Thus, HM should be considered in cirrhotic patients presenting with spastic paraparesis for timely management and improved outcomes. Worldwide approximately 2.5% of patients with cirrhosis are affected with HM. We present a case of a patient with cirrhosis status-post TIPSS who was thought to have hepatic encephalopathy but was found to have HM.
Case Description/Methods: A 42-year-old woman with a history of alcohol-related cirrhosis, hepatitis C, and TIPSS procedure presented with progressive gait abnormalities, slurred speech, and confusion in the background of non-compliance with medications, including lactulose. Her vitals were normal on presentation. Neurological examination revealed upper and lower motor neuron signs: spasticity, hyperreflexia, fasciculations, and a flapping tremor. MRI brain findings were unremarkable for acute pathology, while CT abdomen confirmed cirrhosis and patent TIPSS. With elevated ammonia levels (168 μmol/L), a diagnosis of hepatic myelopathy (HM) was considered. Treatment focused on lactulose and rifaximin led to rapid improvement: spasticity and fasciculations diminished, and cognitive function restored. Discharged stable after three days, the rapid response to treatment with lactulose and the resolution of neurological findings made hepatic myelopathy the most likely diagnosis.
Discussion: HM diagnosis requires the exclusion of other causes of spastic paraparesis and typically presents in the setting of recurrent hepatic encephalopathy. Pathophysiology involves toxin accumulation, particularly ammonia, leading to astrocyte swelling and demyelination of the corticospinal tract. While non-pyramidal symptoms can be reversible with treatment, spastic paraparesis may not always respond. Liver transplant is considered a definitive treatment, but outcomes vary. Early intervention and monitoring of ammonia levels in patients with known portosystemic shunts may reduce irreversible HM cases. Recognizing HM in patients with spastic paraparesis and liver disease is crucial for timely intervention and potentially reversible outcomes. Despite its low prevalence, HM significantly impacts patient morbidity and quality of life, necessitating a comprehensive understanding of its clinical manifestations and management strategies.
Disclosures:
Ishan Kirti, MBBS1, Matthew Lynberg, BS2, Haider A. Naqvi, MD3, Nahar Saleh, MD4. P3135 - Liver Meets Legs: Unraveling Hepatic Myelopathy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Ishan Kirti, MBBS1, Matthew Lynberg, BS2, Haider A. Naqvi, MD3, Nahar Saleh, MD4
1MedStar Union Memorial Hospital, Towson, MD; 2Georgetown University School of Medicine, Washington, DC; 3MedStar Franklin Square Medical Center, Rossville, MD; 4MedStar Union Memorial Hospital, Baltimore, MD
Introduction: Hepatic myelopathy (HM) is a rare neurological complication typically associated with cirrhosis, often manifesting as progressive spastic paraparesis. It presents a diagnostic challenge due to its rarity and varied clinical presentation. Thus, HM should be considered in cirrhotic patients presenting with spastic paraparesis for timely management and improved outcomes. Worldwide approximately 2.5% of patients with cirrhosis are affected with HM. We present a case of a patient with cirrhosis status-post TIPSS who was thought to have hepatic encephalopathy but was found to have HM.
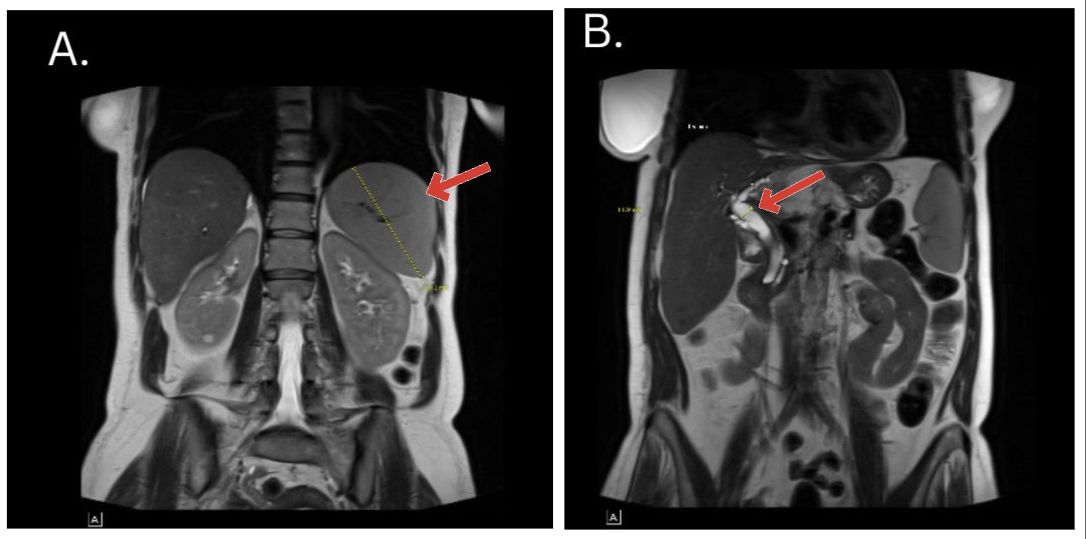
Case Description/Methods: A 42-year-old woman with a history of alcohol-related cirrhosis, hepatitis C, and TIPSS procedure presented with progressive gait abnormalities, slurred speech, and confusion in the background of non-compliance with medications, including lactulose. Her vitals were normal on presentation. Neurological examination revealed upper and lower motor neuron signs: spasticity, hyperreflexia, fasciculations, and a flapping tremor. MRI brain findings were unremarkable for acute pathology, while CT abdomen confirmed cirrhosis and patent TIPSS. With elevated ammonia levels (168 μmol/L), a diagnosis of hepatic myelopathy (HM) was considered. Treatment focused on lactulose and rifaximin led to rapid improvement: spasticity and fasciculations diminished, and cognitive function restored. Discharged stable after three days, the rapid response to treatment with lactulose and the resolution of neurological findings made hepatic myelopathy the most likely diagnosis.
Discussion: HM diagnosis requires the exclusion of other causes of spastic paraparesis and typically presents in the setting of recurrent hepatic encephalopathy. Pathophysiology involves toxin accumulation, particularly ammonia, leading to astrocyte swelling and demyelination of the corticospinal tract. While non-pyramidal symptoms can be reversible with treatment, spastic paraparesis may not always respond. Liver transplant is considered a definitive treatment, but outcomes vary. Early intervention and monitoring of ammonia levels in patients with known portosystemic shunts may reduce irreversible HM cases. Recognizing HM in patients with spastic paraparesis and liver disease is crucial for timely intervention and potentially reversible outcomes. Despite its low prevalence, HM significantly impacts patient morbidity and quality of life, necessitating a comprehensive understanding of its clinical manifestations and management strategies.
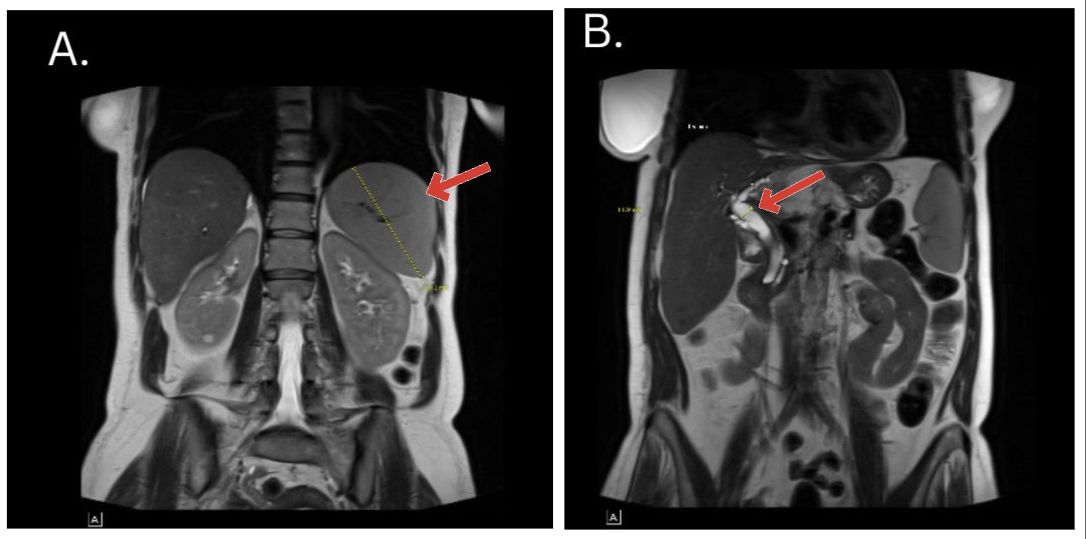
Figure: Fig A. Splenomegaly as a result of liver cirrhosis associated portal hypertension
Fig B. Portal vein dilation in setting of liver cirrhosis
Fig B. Portal vein dilation in setting of liver cirrhosis
Disclosures:
Ishan Kirti indicated no relevant financial relationships.
Matthew Lynberg indicated no relevant financial relationships.
Haider Naqvi indicated no relevant financial relationships.
Nahar Saleh indicated no relevant financial relationships.
Ishan Kirti, MBBS1, Matthew Lynberg, BS2, Haider A. Naqvi, MD3, Nahar Saleh, MD4. P3135 - Liver Meets Legs: Unraveling Hepatic Myelopathy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.

