Monday Poster Session
Category: Small Intestine
P3188 - Risk Factors, Clinical Features and Diagnostic Workup of Sclerosing Mesenteritis: A Single-Center Retrospective Study of 222 Patients
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Bibek Saha, MD
Mayo Clinic
Rochester, MN
Presenting Author(s)
Bibek Saha, MD, Anjali Rajagopal, MBBS, June Tome, MD, Ross Dierkhising, MS, Darrell S. Pardi, MD, MS, Xiao Jing (Iris) Wang, MD
Mayo Clinic, Rochester, MN
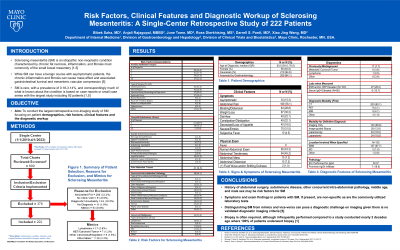
Introduction: Sclerosing mesenteritis (SM) is an idiopathic non-neoplastic condition characterized by chronic fat necrosis, inflammation, and fibrosis of the small bowel mesentery, which can be complicated by gastrointestinal luminal and mesenteric vascular compression. SM is rare, with a prevalence of 0.18-3.14%, and correspondingly much of what is known about the condition is based on case reports or small case series. We present the largest retrospective non-imaging study of SM focusing on demographics, risk factors, clinical features and the diagnostic workup.
Methods: After protocol approval by the Institutional Review Board, a retrospective chart review for SM was performed at our institution between 1/1/2010-6/30/2023. Specifically, 600 charts were subjected to inclusion criteria including adequate follow-up and accurate diagnosis. Descriptive statistics were calculated to summarize characteristics.
Results: A total of 222 cases were included. The median (IQR) age at diagnosis was 63 (54,70), with a male predominance (59.5%) and 94.6% white race (Table 1). Associated factors included history of abdominal surgery (64%), concurrent intra-abdominal pathology (44.1%), autoimmune disease (31.1%), irritable bowel syndrome diagnosis (20.3%) and malignancy (14.4%). While 15.3% of cases were asymptomatic, common symptoms included abdominal pain (76.1%) and nausea/emesis (31.5%). In 47% of cases, symptoms were not clearly related to SM. While 43.3% of patients had a normal abdominal exam, the most common finding was abdominal tenderness (45.2%) with only 7.2% having an abdominal mass. A minority (7.7%) of SM cases were initially misdiagnosed for another condition, primarily metastatic carcinoid tumor but showed SM on biopsy. Conversely, 53 of the original 600 cases were excluded for alternative diagnosis, most commonly lymphoma (2.8%). CT was the initial diagnostic modality in 90.1% of cases, and 41.4% underwent biopsy (image-guided=12.6%, laparoscopic=18% and by laparotomy=10.8%) for definitive diagnosis. Of 56 cases who had serum IgG4 measured, 89.3% were normal. Similarly, of the 37 cases that underwent IgG4 staining, 7 had a prominent IgG4 infiltrate on pathology.
Discussion: History of abdominal surgery, autoimmune disease, other concurrent intra-abdominal pathology, middle age, and male sex may be risk factors for SM. Symptoms and exam findings in patients with SM, if present, are non-specific. Imaging is used for diagnosis, but biopsy is often required.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Bibek Saha, MD, Anjali Rajagopal, MBBS, June Tome, MD, Ross Dierkhising, MS, Darrell S. Pardi, MD, MS, Xiao Jing (Iris) Wang, MD. P3188 - Risk Factors, Clinical Features and Diagnostic Workup of Sclerosing Mesenteritis: A Single-Center Retrospective Study of 222 Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Mayo Clinic, Rochester, MN
Introduction: Sclerosing mesenteritis (SM) is an idiopathic non-neoplastic condition characterized by chronic fat necrosis, inflammation, and fibrosis of the small bowel mesentery, which can be complicated by gastrointestinal luminal and mesenteric vascular compression. SM is rare, with a prevalence of 0.18-3.14%, and correspondingly much of what is known about the condition is based on case reports or small case series. We present the largest retrospective non-imaging study of SM focusing on demographics, risk factors, clinical features and the diagnostic workup.
Methods: After protocol approval by the Institutional Review Board, a retrospective chart review for SM was performed at our institution between 1/1/2010-6/30/2023. Specifically, 600 charts were subjected to inclusion criteria including adequate follow-up and accurate diagnosis. Descriptive statistics were calculated to summarize characteristics.
Results: A total of 222 cases were included. The median (IQR) age at diagnosis was 63 (54,70), with a male predominance (59.5%) and 94.6% white race (Table 1). Associated factors included history of abdominal surgery (64%), concurrent intra-abdominal pathology (44.1%), autoimmune disease (31.1%), irritable bowel syndrome diagnosis (20.3%) and malignancy (14.4%). While 15.3% of cases were asymptomatic, common symptoms included abdominal pain (76.1%) and nausea/emesis (31.5%). In 47% of cases, symptoms were not clearly related to SM. While 43.3% of patients had a normal abdominal exam, the most common finding was abdominal tenderness (45.2%) with only 7.2% having an abdominal mass. A minority (7.7%) of SM cases were initially misdiagnosed for another condition, primarily metastatic carcinoid tumor but showed SM on biopsy. Conversely, 53 of the original 600 cases were excluded for alternative diagnosis, most commonly lymphoma (2.8%). CT was the initial diagnostic modality in 90.1% of cases, and 41.4% underwent biopsy (image-guided=12.6%, laparoscopic=18% and by laparotomy=10.8%) for definitive diagnosis. Of 56 cases who had serum IgG4 measured, 89.3% were normal. Similarly, of the 37 cases that underwent IgG4 staining, 7 had a prominent IgG4 infiltrate on pathology.
Discussion: History of abdominal surgery, autoimmune disease, other concurrent intra-abdominal pathology, middle age, and male sex may be risk factors for SM. Symptoms and exam findings in patients with SM, if present, are non-specific. Imaging is used for diagnosis, but biopsy is often required.
Note: The table for this abstract can be viewed in the ePoster Gallery section of the ACG 2024 ePoster Site or in The American Journal of Gastroenterology's abstract supplement issue, both of which will be available starting October 27, 2024.
Disclosures:
Bibek Saha indicated no relevant financial relationships.
Anjali Rajagopal indicated no relevant financial relationships.
June Tome indicated no relevant financial relationships.
Ross Dierkhising indicated no relevant financial relationships.
Darrell Pardi: AbbVie – Consultant. Applied molecular transport – Grant/Research Support. Finch – Grant/Research Support. Immunic – Consultant. Otsuka – Consultant. Pfizer – Grant/Research Support. Phantom Pharmaceuticals – Consultant. Seres – Consultant, Grant/Research Support. Takeda – Grant/Research Support. Vedanta – Consultant, Grant/Research Support.
Xiao Jing (Iris) Wang indicated no relevant financial relationships.
Bibek Saha, MD, Anjali Rajagopal, MBBS, June Tome, MD, Ross Dierkhising, MS, Darrell S. Pardi, MD, MS, Xiao Jing (Iris) Wang, MD. P3188 - Risk Factors, Clinical Features and Diagnostic Workup of Sclerosing Mesenteritis: A Single-Center Retrospective Study of 222 Patients, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
