Monday Poster Session
Category: Small Intestine
P3238 - Duodenal Diverticulitis Resulting in Gastric Outlet Obstruction
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- RS
Robinderpal Sandhu, DO
Mount Sinai Morningside, Icahn School of Medicine at Mount Sinai
New York, NY
Presenting Author(s)
Adam Tillowitz, MD1, Robinderpal Sandhu, DO2, Michael S.. Smith, MD, MBA3
1Icahn School of Medicine at Mount Sinai Morningside/West, New York, NY; 2Mount Sinai Morningside, Icahn School of Medicine at Mount Sinai, New York, NY; 3Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Gastric Outlet Obstruction (GOO) is a clinical syndrome characterized by epigastric abdominal pain and postprandial vomiting due to mechanical obstruction. The predominant etiology of GOO has changed over the past several decades, from peptic stricturing to malignancy. Duodenal strictures similarly have multiple potential causes, from acid-peptic disease to inflammation and malignancy. We present a rare case of benign GOO secondary to unresolved duodenal diverticulitis and subsequent stricture formation.
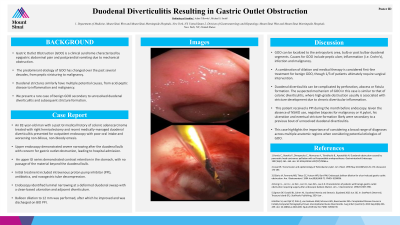
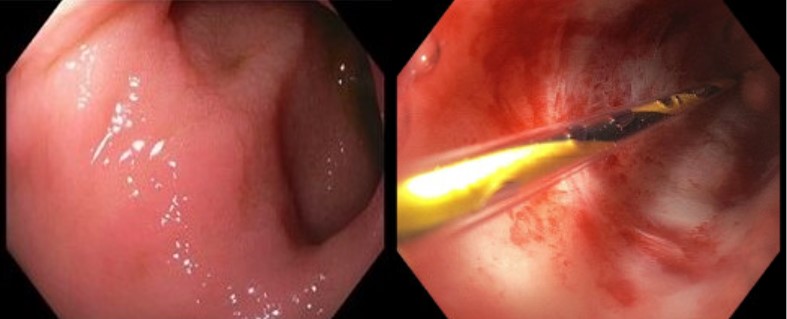
Case Description/Methods: An 82-year-old man with a past GI medical history of colonic adenocarcinoma treated with right hemicolectomy and recent medically-managed duodenal diverticulitis presented for outpatient endoscopy with poor oral intake and worsening non-bilious, non-bloody emesis. Upper endoscopy demonstrated severe narrowing after the duodenal bulb with concern for gastric outlet obstruction, leading to hospital admission. An upper GI series demonstrated contrast retention in the stomach, with no passage of the material beyond the duodenal bulb. Initial treatment included intravenous proton pump inhibitor (PPI), antibiotics, and nasogastric tube decompression. Endoscopy identified luminal narrowing at a deformed duodenal sweep with a clean-based ulceration and adjacent diverticulum. Balloon dilation to 12 mm was performed, after which he improved and was discharged on BID PPI.
Discussion: GOO can be localized to the antropyloric area, bulb or post bulbar duodenal segments. Causes for GOO include peptic ulcer, inflammation (i.e. Crohn’s), infection and malignancy. A combination of dilation and medical therapy is considered first-line treatment for benign GOO, though 1/3 of patients ultimately require surgical intervention.
Duodenal diverticulitis can be complicated by perforation, abscess or fistula formation. The suspected mechanism of GOO in this case is similar to that of colonic diverticulitis, where high-grade obstruction usually is associated with stricture development due to chronic diverticular inflammation. This patient received a PPI during the month before endoscopy. Given the absence of NSAID use, negative biopsies for malignancy or H.pylori, his ulceration and eventual stricture formation likely were secondary to a previous bout of unresolved duodenal diverticulitis. This case highlights the importance of considering a broad range of diagnoses across multiple anatomic regions when considering potential etiologies of GOO.
Disclosures:
Adam Tillowitz, MD1, Robinderpal Sandhu, DO2, Michael S.. Smith, MD, MBA3. P3238 - Duodenal Diverticulitis Resulting in Gastric Outlet Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
1Icahn School of Medicine at Mount Sinai Morningside/West, New York, NY; 2Mount Sinai Morningside, Icahn School of Medicine at Mount Sinai, New York, NY; 3Icahn School of Medicine at Mount Sinai, New York, NY
Introduction: Gastric Outlet Obstruction (GOO) is a clinical syndrome characterized by epigastric abdominal pain and postprandial vomiting due to mechanical obstruction. The predominant etiology of GOO has changed over the past several decades, from peptic stricturing to malignancy. Duodenal strictures similarly have multiple potential causes, from acid-peptic disease to inflammation and malignancy. We present a rare case of benign GOO secondary to unresolved duodenal diverticulitis and subsequent stricture formation.
Case Description/Methods: An 82-year-old man with a past GI medical history of colonic adenocarcinoma treated with right hemicolectomy and recent medically-managed duodenal diverticulitis presented for outpatient endoscopy with poor oral intake and worsening non-bilious, non-bloody emesis. Upper endoscopy demonstrated severe narrowing after the duodenal bulb with concern for gastric outlet obstruction, leading to hospital admission. An upper GI series demonstrated contrast retention in the stomach, with no passage of the material beyond the duodenal bulb. Initial treatment included intravenous proton pump inhibitor (PPI), antibiotics, and nasogastric tube decompression. Endoscopy identified luminal narrowing at a deformed duodenal sweep with a clean-based ulceration and adjacent diverticulum. Balloon dilation to 12 mm was performed, after which he improved and was discharged on BID PPI.
Discussion: GOO can be localized to the antropyloric area, bulb or post bulbar duodenal segments. Causes for GOO include peptic ulcer, inflammation (i.e. Crohn’s), infection and malignancy. A combination of dilation and medical therapy is considered first-line treatment for benign GOO, though 1/3 of patients ultimately require surgical intervention.
Duodenal diverticulitis can be complicated by perforation, abscess or fistula formation. The suspected mechanism of GOO in this case is similar to that of colonic diverticulitis, where high-grade obstruction usually is associated with stricture development due to chronic diverticular inflammation. This patient received a PPI during the month before endoscopy. Given the absence of NSAID use, negative biopsies for malignancy or H.pylori, his ulceration and eventual stricture formation likely were secondary to a previous bout of unresolved duodenal diverticulitis. This case highlights the importance of considering a broad range of diagnoses across multiple anatomic regions when considering potential etiologies of GOO.
Figure: A. Duodenal Diverticulum B. Dilation of Duodenum
Disclosures:
Adam Tillowitz indicated no relevant financial relationships.
Robinderpal Sandhu indicated no relevant financial relationships.
Michael Smith: Castle Biosciences – Advisory Committee/Board Member, Consultant. CDx Diagnostics – Consultant. Lucid Diagnostics – Advisory Committee/Board Member, Consultant. Provation Medical – Consultant. Steris Endoscopy – Advisory Committee/Board Member, Consultant.
Adam Tillowitz, MD1, Robinderpal Sandhu, DO2, Michael S.. Smith, MD, MBA3. P3238 - Duodenal Diverticulitis Resulting in Gastric Outlet Obstruction, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
