Monday Poster Session
Category: Small Intestine
P3246 - Pseudomelanosis Duodeni in a Kidney Transplant Patient
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Mohammad Abudalou, MBBS
University of Missouri School of Medicine
Columbia, MO
Presenting Author(s)
Mohammad Abudalou, MBBS, Mahmoud Mansour, MBBS, Ahmed Swi, MBBS
University of Missouri School of Medicine, Columbia, MO
Introduction: Pseudomelanosis Duodeni (PD) represents a distinctive benign condition, akin to melanosis coli, albeit localized in the duodenum and driven by a different pathogenic mechanism. It is characterized by the accumulation of iron deposits and other substances within the macrophages of the duodenal lamina propria. While PD is an uncommon finding, its clinical significance lies in its association with various medical conditions and medications. In this report, we elucidate a case highlighting the emergence of PD after kidney transplantation, shedding light on its diagnostic and clinical nuances.
Case Description/Methods: A 69-year-old Hispanic male, with a medical history significant for hepatitis C-induced cirrhosis and end-stage renal disease secondary to uncontrolled type 2 diabetes, presented with complaints of epigastric pain. He had undergone orthotopic liver transplant in 2000 and subsequently underwent kidney transplantation in 2021. His medication regimen included immunosuppressants and cardiovascular drugs such as tacrolimus, mycophenolic acid, hydralazine, nifedipine, insulin, atorvastatin and clopidogrel.
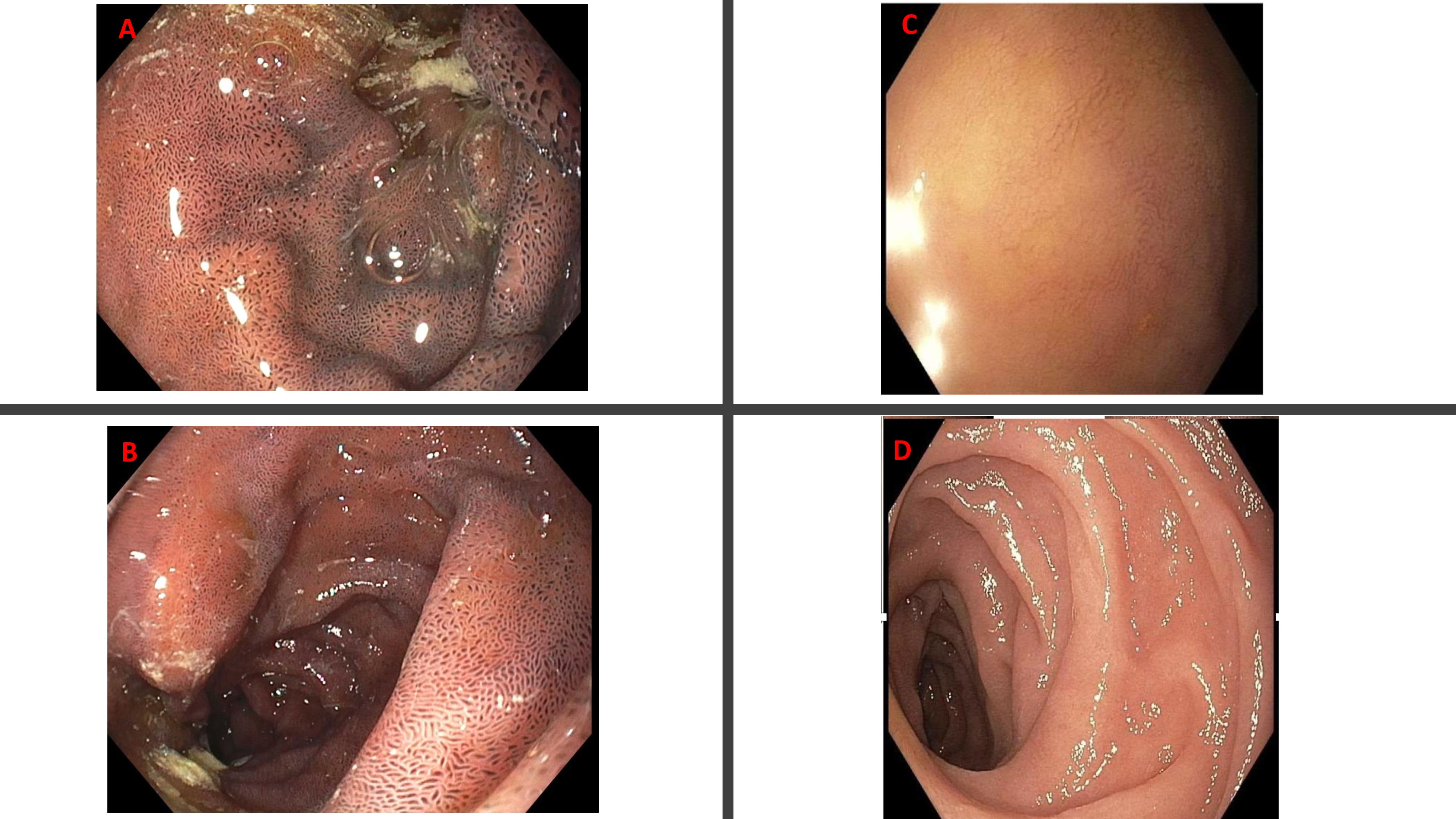
During Esophagogastroduodenoscopy (EGD), a normal esophagus and mild antral erythema were observed. However, the first and second part of duodenum exhibited a pattern of black dotted mucosal pigmentation (Figure A, B), contrasting with previous examinations showing a normal duodenal mucosa right before patient’s renal transplant (Figure C,D).
Biopsies taken from the duodenal mucosa revealed the presence of pseudomelanosis duodeni (PD), characterized by the accumulation of iron deposits in duodenal lamina propria macrophages.
Discussion: PD's pathogenesis remains incompletely understood, though it has been associated with conditions such as hypertension, end-stage renal disease, and diabetes, as well as certain medications like sulfa-containing diuretics, Hydralazine, and iron supplements. Noteworthy is its occurrence in patients post-renal transplant, as evidenced in our case, where the duodenal mucosa remained unaffected prior to transplantation. The benign nature of PD obviates the necessity for histological confirmation, with diagnosis primarily reliant on endoscopic appearance. Our case underscores the importance of vigilance for PD in post-transplant patients, underscoring its evolving clinical spectrum and necessitating further research into its pathogenesis and implications.
Disclosures:
Mohammad Abudalou, MBBS, Mahmoud Mansour, MBBS, Ahmed Swi, MBBS. P3246 - Pseudomelanosis Duodeni in a Kidney Transplant Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
University of Missouri School of Medicine, Columbia, MO
Introduction: Pseudomelanosis Duodeni (PD) represents a distinctive benign condition, akin to melanosis coli, albeit localized in the duodenum and driven by a different pathogenic mechanism. It is characterized by the accumulation of iron deposits and other substances within the macrophages of the duodenal lamina propria. While PD is an uncommon finding, its clinical significance lies in its association with various medical conditions and medications. In this report, we elucidate a case highlighting the emergence of PD after kidney transplantation, shedding light on its diagnostic and clinical nuances.
Case Description/Methods: A 69-year-old Hispanic male, with a medical history significant for hepatitis C-induced cirrhosis and end-stage renal disease secondary to uncontrolled type 2 diabetes, presented with complaints of epigastric pain. He had undergone orthotopic liver transplant in 2000 and subsequently underwent kidney transplantation in 2021. His medication regimen included immunosuppressants and cardiovascular drugs such as tacrolimus, mycophenolic acid, hydralazine, nifedipine, insulin, atorvastatin and clopidogrel.
During Esophagogastroduodenoscopy (EGD), a normal esophagus and mild antral erythema were observed. However, the first and second part of duodenum exhibited a pattern of black dotted mucosal pigmentation (Figure A, B), contrasting with previous examinations showing a normal duodenal mucosa right before patient’s renal transplant (Figure C,D).
Biopsies taken from the duodenal mucosa revealed the presence of pseudomelanosis duodeni (PD), characterized by the accumulation of iron deposits in duodenal lamina propria macrophages.
Discussion: PD's pathogenesis remains incompletely understood, though it has been associated with conditions such as hypertension, end-stage renal disease, and diabetes, as well as certain medications like sulfa-containing diuretics, Hydralazine, and iron supplements. Noteworthy is its occurrence in patients post-renal transplant, as evidenced in our case, where the duodenal mucosa remained unaffected prior to transplantation. The benign nature of PD obviates the necessity for histological confirmation, with diagnosis primarily reliant on endoscopic appearance. Our case underscores the importance of vigilance for PD in post-transplant patients, underscoring its evolving clinical spectrum and necessitating further research into its pathogenesis and implications.
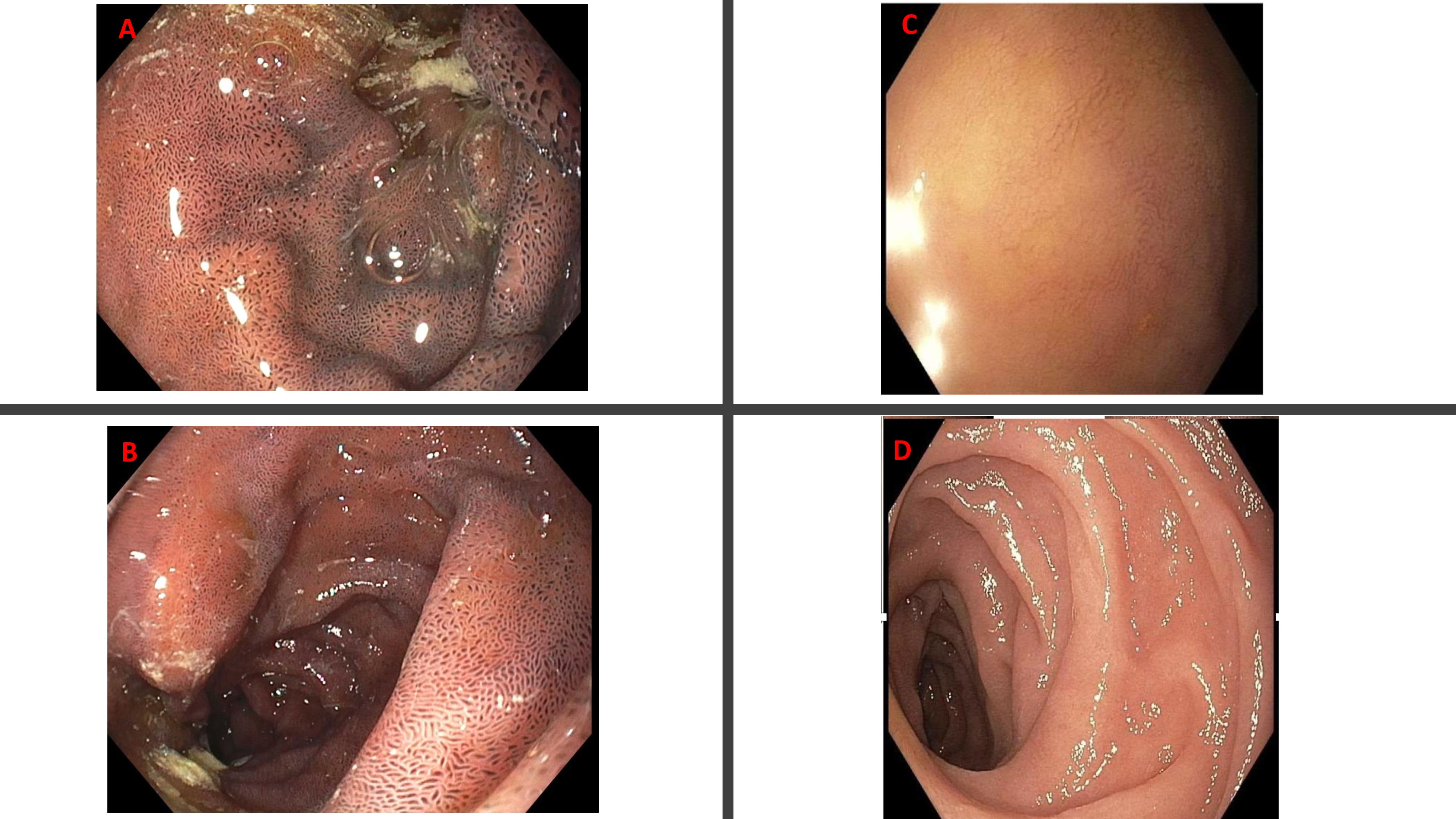
Figure: A: black dotted mucosa in first part of duodenum B: black dotted mucosa in second part of duodenum C: normal first part of duodenum D: normal second part of duodenum.
Disclosures:
Mohammad Abudalou indicated no relevant financial relationships.
Mahmoud Mansour indicated no relevant financial relationships.
Ahmed Swi indicated no relevant financial relationships.
Mohammad Abudalou, MBBS, Mahmoud Mansour, MBBS, Ahmed Swi, MBBS. P3246 - Pseudomelanosis Duodeni in a Kidney Transplant Patient, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
