Monday Poster Session
Category: Small Intestine
P3259 - Splenic Marginal Zone Lymphoma Manifesting as Acquired Angioedema of the Small Intestine
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio

Samuel Addo, MD
UNC Health Blue Ridge
Morganton, NC
Presenting Author(s)
Award: Presidential Poster Award
Samuel Addo, MD1, Madeline Durairaj, MD1, Mohamed O. Seisa, MD1, Claire R. Rinaldo, BS, DO2, Suneel Mohammed, MD1
1UNC Health Blue Ridge, Morganton, NC; 2UNC Health Blue Ridge, Denver, NC
Introduction: Acquired angioedema (AAE) is a rare but potentially life threatening condition characterized by recurrent non-pitting, non-pruritic swelling due to excess bradykinin levels. It is often associated with deficiencies in C1 esterase inhibitor (C1INH), which can result from autoantibodies or immune complex mediated degradation secondary to underlying lymphoproliferative or autoimmune disorders. We present a case of splenic marginal zone lymphoma (SMZL) manifesting as recurrent angioedema of the small intestine.
Case Description/Methods: A 73-year-old female with history of type II diabetes, hypertension presented to the ER with recurrent episodes of sudden facial swelling and epigastric pain, marking her fourth angioedema episode in eight months. Onset typically involved neck and facial tightness followed by swelling of the tongue, throat, and lips, accompanied by dysphagia, hoarseness, shortness of breath, severe abdominal pain, nausea, vomiting and diarrhea. She denied triggers like infection, medication or supplement use.
There was no history of skin rashes or pruritis. Two years earlier, she was referred for asymptomatic lymphocytosis evaluation, with concern for chronic lymphocytic leukemia, although patient declined further investigation.
On examination, the patient was tachycardic, and tachypneic. Facial swelling was noted along with swelling of the tongue and lips. Diffuse abdominal tenderness was noted along with moderate splenomegaly.
Labs revealed leukocytosis with lymphocytic predominance and atypical lymphocyte, and decreased complement levels (C1 esterase inhibitor protein, C1q, and C4). CT abdomen and pelvis showed large hiatal with gastric, duodenal and distal small bowel wall thickening with splenomegaly and lymphadenopathy.
EGD identified gastric antral erythema with chronic gastritis and foveolar hyperplasia. Bone marrow biopsy confirmed splenic marginal zone lymphoma (SMZL). The patient was managed acutely with fresh frozen plasma with subsequent management included chemotherapy, berotralstat, conestat alpha, and icatibant.
Discussion: This case hightlights the need of investigating underlying disorders in elderly patients with new or recurrent intestinal angioedema. Clinicians should be vigilant in adults over 40 with no familial angioedema history. Key diagnostics include complement levels (low C1q and C4), abdominal imaging and history. Management involves addressing the underlying disorder, and providing symptomatic relief during acute attacks, and preventing recurrences.
Disclosures:
Samuel Addo, MD1, Madeline Durairaj, MD1, Mohamed O. Seisa, MD1, Claire R. Rinaldo, BS, DO2, Suneel Mohammed, MD1. P3259 - Splenic Marginal Zone Lymphoma Manifesting as Acquired Angioedema of the Small Intestine, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Samuel Addo, MD1, Madeline Durairaj, MD1, Mohamed O. Seisa, MD1, Claire R. Rinaldo, BS, DO2, Suneel Mohammed, MD1
1UNC Health Blue Ridge, Morganton, NC; 2UNC Health Blue Ridge, Denver, NC
Introduction: Acquired angioedema (AAE) is a rare but potentially life threatening condition characterized by recurrent non-pitting, non-pruritic swelling due to excess bradykinin levels. It is often associated with deficiencies in C1 esterase inhibitor (C1INH), which can result from autoantibodies or immune complex mediated degradation secondary to underlying lymphoproliferative or autoimmune disorders. We present a case of splenic marginal zone lymphoma (SMZL) manifesting as recurrent angioedema of the small intestine.
Case Description/Methods: A 73-year-old female with history of type II diabetes, hypertension presented to the ER with recurrent episodes of sudden facial swelling and epigastric pain, marking her fourth angioedema episode in eight months. Onset typically involved neck and facial tightness followed by swelling of the tongue, throat, and lips, accompanied by dysphagia, hoarseness, shortness of breath, severe abdominal pain, nausea, vomiting and diarrhea. She denied triggers like infection, medication or supplement use.
There was no history of skin rashes or pruritis. Two years earlier, she was referred for asymptomatic lymphocytosis evaluation, with concern for chronic lymphocytic leukemia, although patient declined further investigation.
On examination, the patient was tachycardic, and tachypneic. Facial swelling was noted along with swelling of the tongue and lips. Diffuse abdominal tenderness was noted along with moderate splenomegaly.
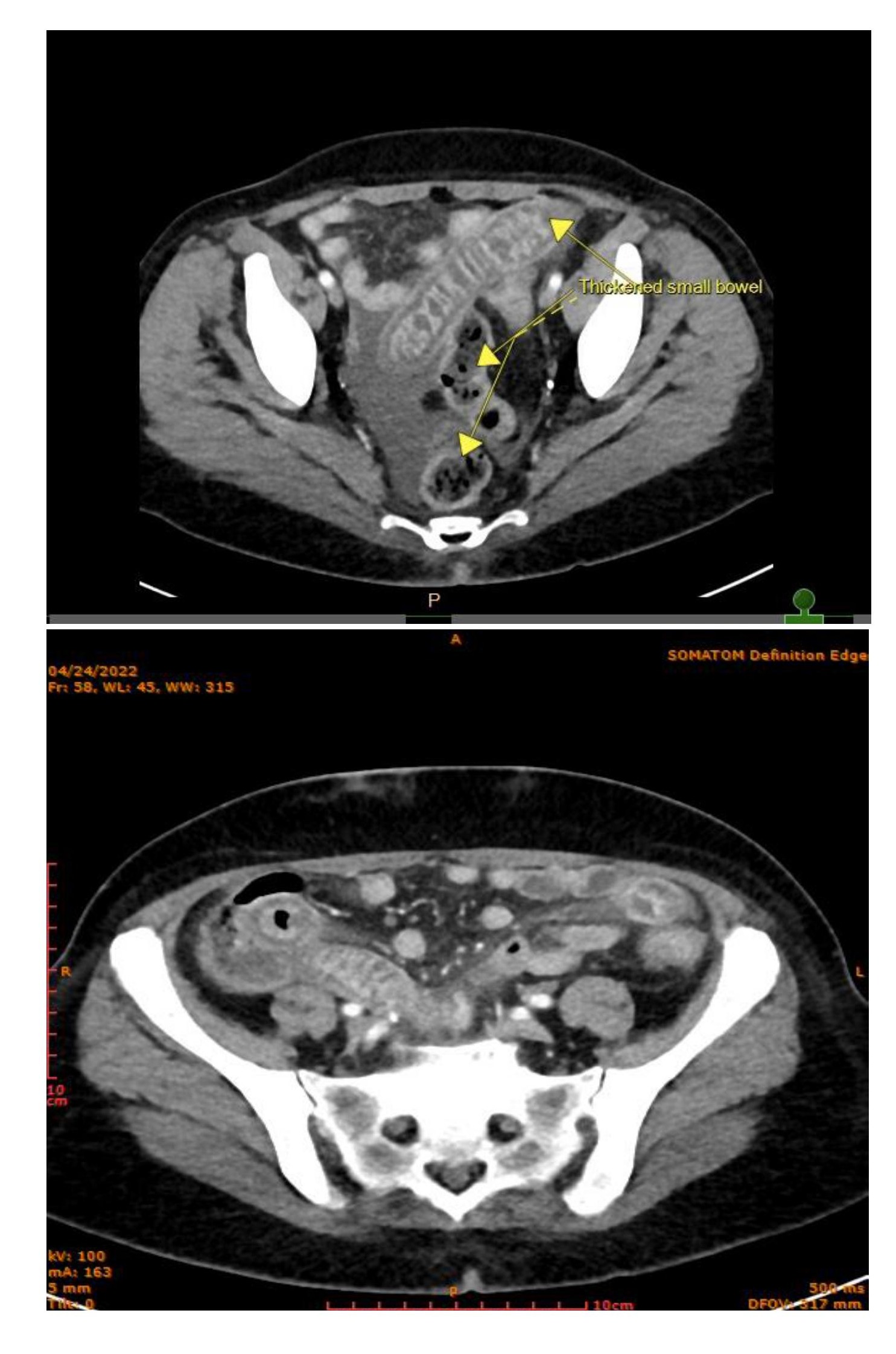
Labs revealed leukocytosis with lymphocytic predominance and atypical lymphocyte, and decreased complement levels (C1 esterase inhibitor protein, C1q, and C4). CT abdomen and pelvis showed large hiatal with gastric, duodenal and distal small bowel wall thickening with splenomegaly and lymphadenopathy.
EGD identified gastric antral erythema with chronic gastritis and foveolar hyperplasia. Bone marrow biopsy confirmed splenic marginal zone lymphoma (SMZL). The patient was managed acutely with fresh frozen plasma with subsequent management included chemotherapy, berotralstat, conestat alpha, and icatibant.
Discussion: This case hightlights the need of investigating underlying disorders in elderly patients with new or recurrent intestinal angioedema. Clinicians should be vigilant in adults over 40 with no familial angioedema history. Key diagnostics include complement levels (low C1q and C4), abdominal imaging and history. Management involves addressing the underlying disorder, and providing symptomatic relief during acute attacks, and preventing recurrences.
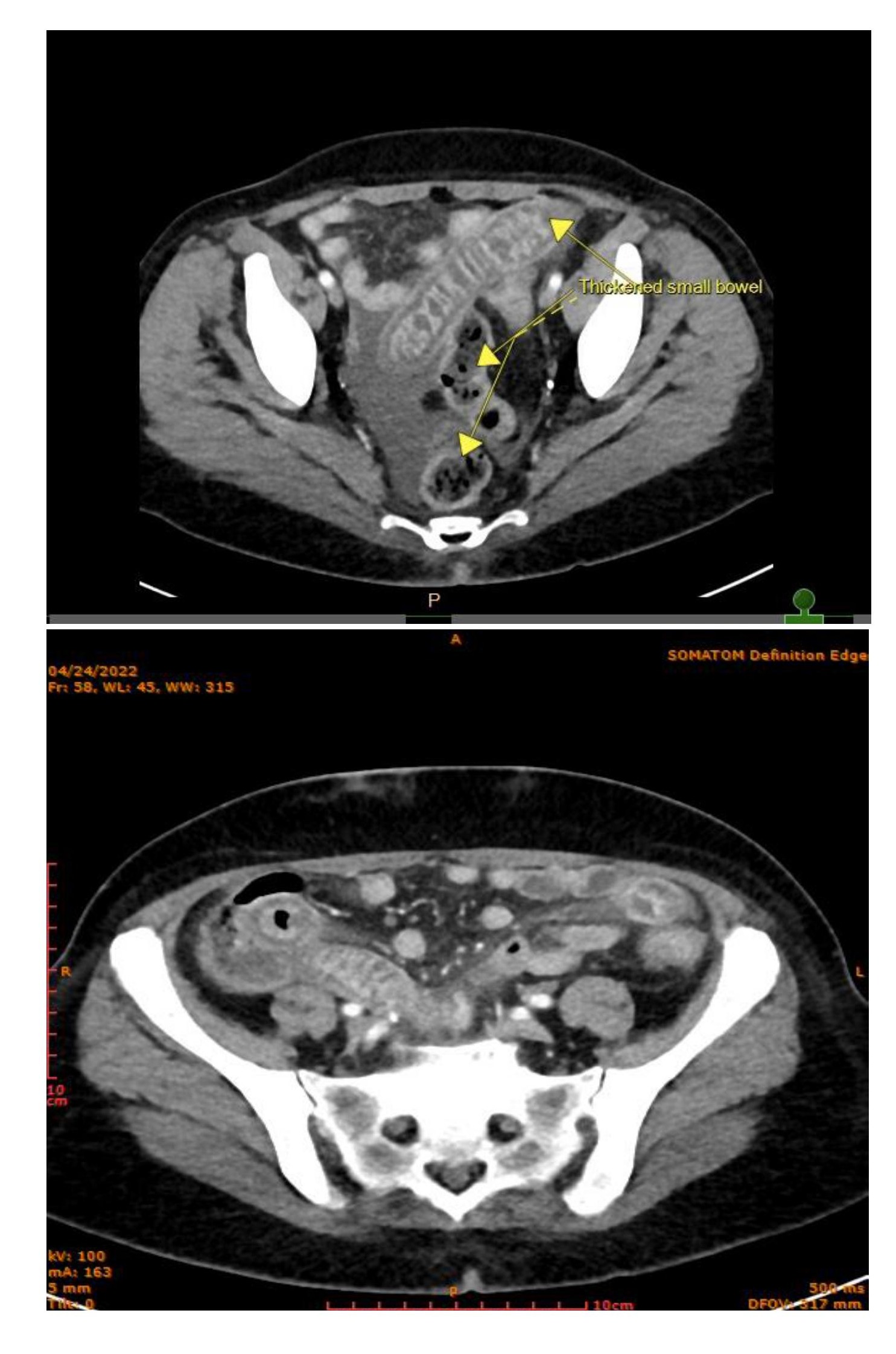
Figure: CT of the abdomen and pelvis showing the terminal ileal wall thickening secondary to inflammation and edema. Severely thickened segment of small bowel in the lower abdomen associated with mesenteric inflammation and edema.
Disclosures:
Samuel Addo indicated no relevant financial relationships.
Madeline Durairaj indicated no relevant financial relationships.
Mohamed Seisa indicated no relevant financial relationships.
Claire Rinaldo indicated no relevant financial relationships.
Suneel Mohammed indicated no relevant financial relationships.
Samuel Addo, MD1, Madeline Durairaj, MD1, Mohamed O. Seisa, MD1, Claire R. Rinaldo, BS, DO2, Suneel Mohammed, MD1. P3259 - Splenic Marginal Zone Lymphoma Manifesting as Acquired Angioedema of the Small Intestine, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.


