Monday Poster Session
Category: Small Intestine
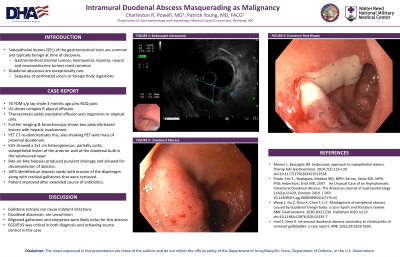
P3302 - Intramural Duodenal Abscess Masquerading as Malignancy
Monday, October 28, 2024
10:30 AM - 4:00 PM ET
Location: Exhibit Hall E
Has Audio
- CP
Charleston R. Powell, MD
Walter Reed National Military Medical Center
Bethesda, MD
Presenting Author(s)
Charleston R. Powell, MD, Patrick E. Young, MD, FACG
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Subepithelial lesions (SEL) of the gastrointestinal tract are common and typically benign at time of discovery. Gastrointestinal stromal tumors, leiomyomas, lipomas, neural and neuroendocrine tumors are of the more commonly encountered SEL.
Duodenal abscesses are exceptionally uncommon. They are usually sequelae of perforated ulcers or less commonly foreign body ingestions. We present an asymptomatic duodenal abscess that was identified through workup for a suspected duodenal malignancy.
Case Description/Methods: A 76-year-old male presented with abdominal pain three months after an uncomplicated laparoscopic cholecystectomy for necrotizing cholecystitis. Abdominal ultrasound revealed a complex, right-sided pleural effusion. Thoracentesis yielded an eosinophilic predominant, exudative effusion without atypical cells or organisms. Bronchoscopy and cross-sectional imaging showed two heterogenous, hypoenhancing pleural lesions with hepatic involvement. PET CT showed hypermetabolism of these masses in addition to a proximal duodenum lesion concerning for a primary malignancy.
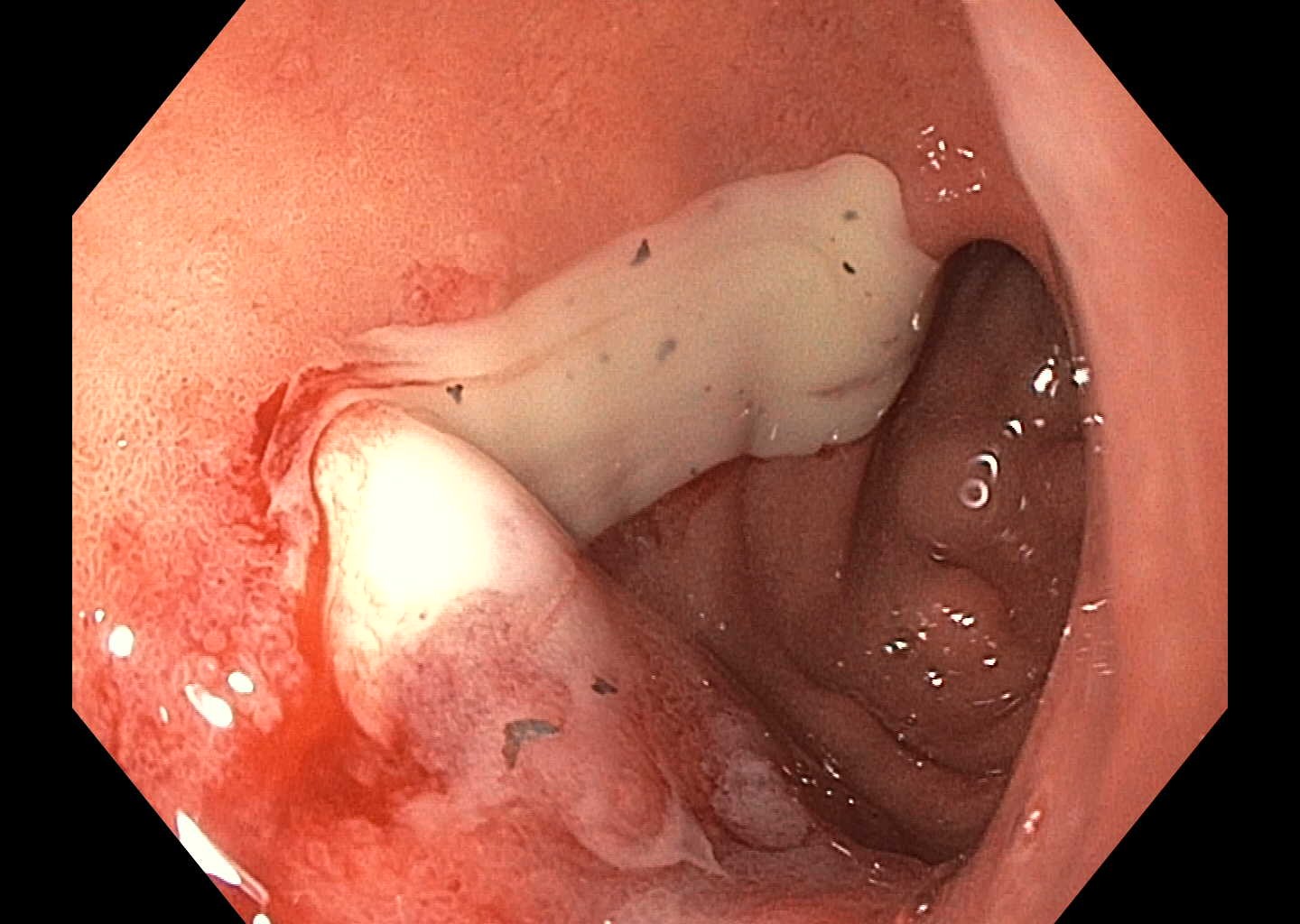
EGD with EUS showed a 2x1 cm heterogeneous, partially cystic, subepithelial lesion of the anterior wall of the duodenal bulb in the submucosal layer. Bite-on-bite biopsies of the lesion induced purulent drainage and the lesion was decompressed completely. Percutaneous biopsy of a hepatic lesion was also performed. Pathology for both duodenal and hepatic lesions showed necroinflammatory debris without neoplasia, consistent with a resolving abscess. Video-assisted thoracoscopic surgery identified an abscess cavity with erosion of the diaphragm along with residual gallstones that were retrieved. The gallstones and pleural biopsy grew E. coli. The patient improved with an extended course of oral antibiotics.
Discussion: This clinical presentation of a duodenal abscess lacked concomitant symptoms expected of such an infection. Gallstone ectopia from spillage has been reported to create indolent infections that do not present clinically for months to years. This patient had gallstone migration into the pleural space resulting in empyema. The nidus for the intramural duodenal abscess is less clear, but local inflammation from ongoing infection is likely. EUS and EGD were instrumental in making a diagnosis as well in achieving source control.
Disclosures:
Charleston R. Powell, MD, Patrick E. Young, MD, FACG. P3302 - Intramural Duodenal Abscess Masquerading as Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Subepithelial lesions (SEL) of the gastrointestinal tract are common and typically benign at time of discovery. Gastrointestinal stromal tumors, leiomyomas, lipomas, neural and neuroendocrine tumors are of the more commonly encountered SEL.
Duodenal abscesses are exceptionally uncommon. They are usually sequelae of perforated ulcers or less commonly foreign body ingestions. We present an asymptomatic duodenal abscess that was identified through workup for a suspected duodenal malignancy.
Case Description/Methods: A 76-year-old male presented with abdominal pain three months after an uncomplicated laparoscopic cholecystectomy for necrotizing cholecystitis. Abdominal ultrasound revealed a complex, right-sided pleural effusion. Thoracentesis yielded an eosinophilic predominant, exudative effusion without atypical cells or organisms. Bronchoscopy and cross-sectional imaging showed two heterogenous, hypoenhancing pleural lesions with hepatic involvement. PET CT showed hypermetabolism of these masses in addition to a proximal duodenum lesion concerning for a primary malignancy.
EGD with EUS showed a 2x1 cm heterogeneous, partially cystic, subepithelial lesion of the anterior wall of the duodenal bulb in the submucosal layer. Bite-on-bite biopsies of the lesion induced purulent drainage and the lesion was decompressed completely. Percutaneous biopsy of a hepatic lesion was also performed. Pathology for both duodenal and hepatic lesions showed necroinflammatory debris without neoplasia, consistent with a resolving abscess. Video-assisted thoracoscopic surgery identified an abscess cavity with erosion of the diaphragm along with residual gallstones that were retrieved. The gallstones and pleural biopsy grew E. coli. The patient improved with an extended course of oral antibiotics.
Discussion: This clinical presentation of a duodenal abscess lacked concomitant symptoms expected of such an infection. Gallstone ectopia from spillage has been reported to create indolent infections that do not present clinically for months to years. This patient had gallstone migration into the pleural space resulting in empyema. The nidus for the intramural duodenal abscess is less clear, but local inflammation from ongoing infection is likely. EUS and EGD were instrumental in making a diagnosis as well in achieving source control.
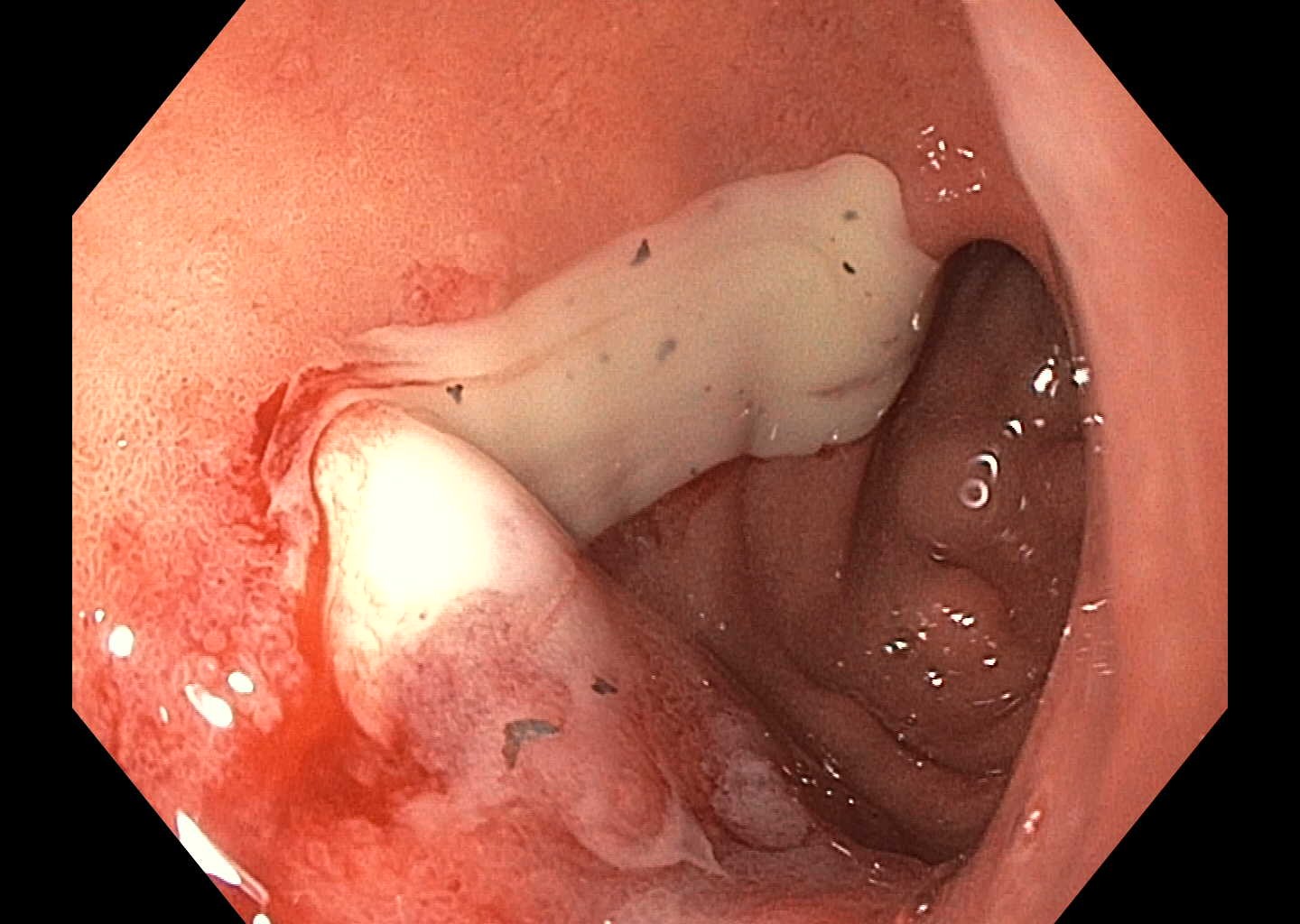
Figure: Duodenal abscess
Disclosures:
Charleston Powell indicated no relevant financial relationships.
Patrick Young indicated no relevant financial relationships.
Charleston R. Powell, MD, Patrick E. Young, MD, FACG. P3302 - Intramural Duodenal Abscess Masquerading as Malignancy, ACG 2024 Annual Scientific Meeting Abstracts. Philadelphia, PA: American College of Gastroenterology.
